Canine Hypothyroidism

Sushant Sadotra Introduction: Hypothyroidism is a prevalent thyroid disorder that is caused due to the deficiency of thyroid hormone. In this condition, there is an irregular short production and improper secretion of thyroid hormones into the blood from the thyroid gland. This leads to a slow metabolic rate and loss of proper body functions. Regarding pet animals, hypothyroidism is mostly occurring among dogs and rarely in cats and other pet animals. Hypothyroidism Etiology in canines: Imbalance at any level of the hypothalamic-pituitary-thyroid axis can cause hypothyroidism in animals, especially dogs. In Adult dogs, the onset of primary hypothyroidism can cause either because of lymphocytic thyroiditis or idiopathic atrophy of the thyroid gland. The gradual destruction of follicles and secondary fibrosis on the gland because of diffuse infiltration by lymphocytes, plasma cells, and macrophages into the thyroid gland. This condition is known as lymphocytic thyroiditis. Loss of thyroid parenchyma leads to the idiopathic atrophy of the thyroid gland, in which fatty tissue will replace the lost thyroid parenchyma. The condition can occur due to autoimmune thyroiditis. Secondary hypothyroidism can be caused due to the damage of pituitary thyrotrophs by tumor growth, leading to the deficiency of one or more pituitary hormones. Hypothyroidism in dogs can occur due to other rare causes such as congenital hypothyroidism or neoplastic destruction of thyroid tissue. Congenital hypothyroidism can be primary or secondary. Thyroid dysgenesis and dyshormonogenesis can cause congenital primary hypothyroidism in dogs. Congenital secondary hypothyroidism can show clinical signs caused by the deficiency of growth hormones such as dwarfism, lethargy, gait abnormalities, or pituitary dwarfism. Diagnosis of hypothyroidism in canines: A variety of nonthyroidal factors and other conditions can mimic thyroid disorder and mislead the correct diagnosis of canine hypothyroidism. The severity and chronicity of the clinical findings associated with hypothyroidism and other clinicopathologic abnormalities of the hypothyroid state can be a basis for the choice of a proper diagnostic test. Tests that could confirm the diagnosis of hypothyroidism in canines are mentioned below: Total T4: The initial screening test for hypothyroidism can determine Total T4 concentration. A dog with a T4 concentration lower than the reference range limits may be anticipated to have a hypothyroid issue. However, it can also indicate that the dog can have a nonthyroidal illness such as sick euthyroid syndrome. Therefore, the total T4 test alone cannot be a proper diagnosis. Free T4: In serum, unbound T4 is supposed to be biologically active. Therefore, it is a very used test to differentiate between hypothyroid and euthyroid dogs. Also, a free T4 assay can give a better diagnosis with high sensitivity and specificity. Most commercial Free T4 tests use the method of single-stage solid phase (analogue) assays. However, an equilibrium dialysis step can improve the accuracy. Free T3: Among T4 and T3, T3 is the most potent hormone in animals. Therefore, measuring Free T3 is also a sensitive diagnostic step. However, during the onset of the primary hypothyroidism, serum T3 determination is weak. Also, it is found that in hypothyroidism dogs, serum T3 concentrations could be low, normal, or high. If the serum concentration of T3 is high, it is to be checked whether or not anti-T3 antibodies are producing false results in the T3 radioimmunoassay. Serum TSH concertation: In primary hypothyroidism, high serum TSH concentrations are expected that further may lead to low serum concentrations of T4 and free T4. A species-specific TSH assay can be used to check the high level of serum TSH. However, a false-negative result showing normal TSH concentrations may indicate a condition of primary hypothyroidism; a false-positive result showing high serum TSH concentrations may indicate a nonthyroidal illness in a euthyroid dog. A normal serum TSH concentration can indicate secondary hypothyroidism in a few cases. Therefore, serum TSH concentration results should always be coupled with other tests for definite confirmations. TSH stimulation test: In this particular test, bovine TSH is introduced exogenously into the dog’s body, and the thyroid gland’s response is evaluated. Firstly, a basal T4 is measured. Then bovine TSH is administrated at a dosage of 0.1 U/kg. After 6 hours, T4 levels are calculated for the second time to check the response of the thyroid gland. Result interpretations could be a no response for hypothyroidism, a normal and blunted response for the sick euthyroid syndrome. Although the TSH stimulation test is one of the accurate tests to check thyroid function, it is expensive and less available. Imaging: Thyroid Ultrasonography can detect the decreased echogenicity followed by decreased thyroid volume. The procedure can take the best imaging of the thyroid gland by technetium 99m (99mTc). This diagnostic tool can differentiate between hypothyroidism and euthyroid sickness. Therapeutic trial: In this approach, a thyroxine supplementation is given to a dog at a particular dosage. If the response is positive, the supplementation is stopped to check for the return of clinical signs related to hypothyroidism. This can confirm that the dog has thyroid-responsive diseases rather than other nonthyroidal issues. However, before starting a therapeutic trial, every attempt should eliminate nonthyroidal sickness. Also, therapeutic monitoring should be performed in case the therapy is unsuccessful. Treatment of hypothyroidism in canines: The typical treatment of hypothyroidism in dogs is the oral medication of levothyroxine (L-T4). L-T4 is a synthetic thyroid hormone that can restore blood thyroid hormone concentrations and reverse hypothyroidism’s effects. The replacement of natural with synthetic hormones will be used for the rest of the animal’s life. However, a great precaution is needed with the initial dose and tailoring of the drug. The dosages of L-T4 in d are 0.01–0.02 mg/lb (0.02–0.04 mg/kg). The drug is given every day once or twice without food. Reference: Hypothyroidism is the Most Common Hormone Imbalance of Dogs; Wendy Brooks, DVM, DABVP. Date Published: 02/26/2002, Date Reviewed/Revised: 08/16/2019. Strey S, Mischke R, Rieder J. Hypothyreose beim Hund: eine Übersicht [Hypothyroidism in dogs: an overview]. Tierarztl Prax Ausg K Kleintiere Heimtiere. 2021 Jun; 49(3):195-205. German. doi: 10.1055/a-1367-3387. Epub 2021 Jun 22. PMID: 34157761 Mark E. Peterson. Hypothyroidism in Animals. Last
Canine Distemper Virus
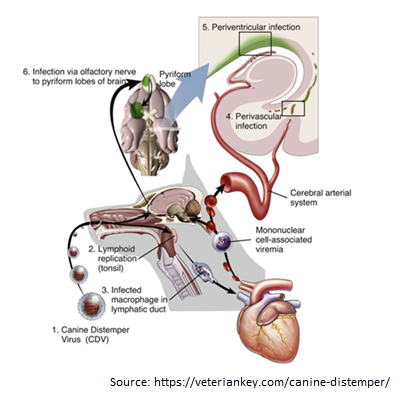
Canine Distemper Virus Tang Nguyen Mai Trinh Infection of canine distemper virus (CDV) is common in most terrestrial carnivores in the wild, especially in the Canidae family (eg, wolves, foxes, domestic dogs, etc.), as well as certain ferrets, otters, raccoons, cats, and even marine animals [1]. CDV is a member of the Paramyxoviridae family which the genus Morbilivirus was first described in the 1970s, however, it was only isolated in 1905 from the nasal secretions of infected dogs by a French veterinarian, [2]. CDV is now known as the most dangerous disease in dogs because of its propensity to infect through respiratory and digestive pathways and cause death in virtually all canines. When infected with it, the unvaccinated host has a 100% mortality rate [3]. Structure of Canine distemper virus CDV is known as a single-stranded RNA virus, like many other viruses CDV has an N nucleocapsid protein that is responsible for genome replication, matrix (M), fusion (F), phosphoprotein (P), and polymerase (L) which are involved in genomic and mRNA transcription. Whereas nonstructural proteins C and V have been identified as virulence factors involved in the modulation of immune responses and innate immunity, proteins like H and F are essential for viral attachment, invasion, and fusion into host cells [4-6]. Transmission Puppies and dogs most often become infected through airborne exposure to the virus from an infected dog or wild animal. CDV enter the dog’s body through respiratory secretions, most notably coughing and sneezing. Virus particles can spread about 25 feet with a single sneeze, then proliferate in immune cells such as macrophages, T and B cells via the SLAM receptor within 24 hours [8] and spreads to tonsils and lymph nodes via the lymphatic vessels, causing long-term immunosuppression [9-11]. The amount of virus in the lymph nodes of the throat, tonsils, and bronchi will go up after 2 to 4 days of infection, and the virus continues to release and replicate in multiple organs. This process takes 4 to 6 days after infection and affects organs such as the thymus, spleen, lymph nodes, stomach cells, lungs, and bone marrow. The increased concentration of virus in the lymph node tissue at this time causes the number of white blood cells to decrease, resulting in the infected dog’s body temperature increasing [12]. The virus begins to migrate to specific epithelium and the central nervous system (CNS) via the blood or CSF after around 8 –10 days [10]. Simultaneously, organs such as the respiratory tract, intestines, and urinary tract begin to experience significant infections as lymphocytes are destroyed, resulting in a massive release of viruses into these organs [13]. Figure 2. The process of entry and replication of CDV in dogs.1, The CDV virus enters the dog’s body through the respiratory tract. 2, the virus begins to multiply in the tonsils, bronchial lymph nodes, oropharyngeal nodes, and gastrointestinal lymphoid tissues. 3, the virus attacks immune cells such as macrophages and is released to other organs such as the heart. 4, The virus enters the central nervous system (CNS) through the circulatory system. 5, Virus enters the cerebrospinal fluid (CFS). 6, Viral migration to the pyramidal lobes of the cerebral cortex through the nasal passages to the central nervous system [14]. Clinical Symptoms of Canine Distemper Virus infection in dogs The CDV virus can cause disease in dogs of any age, although it is more common in pups aged 12 to 16 weeks and in unvaccinated dogs. Because pups’ immune systems are so immature, they are easily infected by the virus if they come into touch with dogs that have already been afflicted with CDV. When the dog get infected with the CDV virus, early symptoms include fever, weariness, lack of appetite, apathy, and a reluctance to be active [9]. However, these symptoms are quite similar to those of the parvovirus, which primarily infects the digestive system, whereas CDV not only assaults the digestive system but also damage to the respiratory system, neurological system, bones, arthritis, eyes, and skin [13]. Prolonged vomiting, diarrhea, severe dehydration, and stool abnormalities in color, consistency, and blood and mucus contribute to gastritis and intestinal inflammation in the early stages. Finally, the dog was unable to defecate, resulting in death (Figure 3A). Pus discharge, ulcers, and progressively becoming clouded eyes can lead to conjunctivitis and even blindness, while the skin appears as spots with pus within, then gradually changes from red to yellow (Figures 3 B and C). Signs such as a runny nose with green mucus in the early stage, shortness of breath in the latter stage, and shortness of breath lead to pneumonia in the respiratory system (Figure 3B). Figure 3. Signs of CDV infection in dogs. A, Dogs have digestive system damage, diarrhea with blood [17]. B, Eyes are damaged causing pus discharge, ulcers, while the nose shows signs of runny nose with green mucus [15]. C, The skin also appears spots that have pus inside. D and E, the dog’s paw and nose epithelium show basal keratinocytes. F, enamel deterioration in adult dogs following neonatal CDV infection [13]. When the disease is severe, evidence of central nervous system damage such as convulsions, hemiplegia, or quadriplegia will occur; at this stage, 99% of infected dogs will die. Furthermore, the CDV virus can attach to lymphocytes and enter the cerebrospinal fluid (CSF), causing harm to the central nervous system. In addition, CDV was discovered in the foot and nasal epithelium, promoting basal keratinocyte growth, which was clearly recognized in the Figures 3D and E. Although CDV infection leads to the above clinical signs, however the appearance of these signs is also dependent on habitat, age, host immunity, and virulence of the virus strain [13]. Studies have also demonstrated that CDV can be passed from mother to puppy through the placenta during pregnancy. When the mother dog is infected with the virus, it can lead to miscarriage, stillbirth, but this depends on the pregnancy stage of the mother dog [16]. For the lucky puppies
Canine Babesiosis
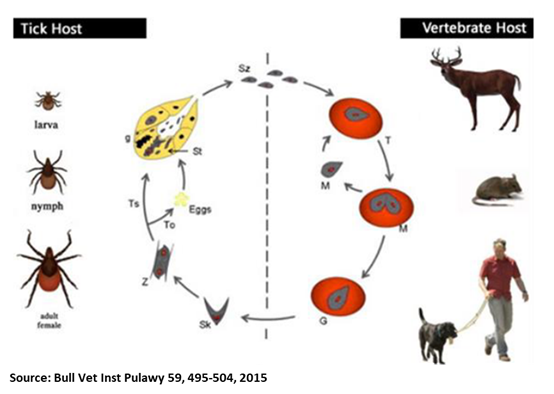
Oliver Organista, LA Canine babesiosis is a tick-borne, protozoal, haemoparasitic disease that can cause varying degrees of haemolytic anaemia, splenomegaly, thrombocytopenia and fever. It is very endemic to different parts of the world, and presents varying clinical, hematological, and pathological manifestation depending on the species and subspecies involved.1,2 There are two hosts for the transmission of Babesia spp., viz. invertebrate (tick) and vertebrate host. Dogs are one among the many targets of Babesia spp., causing canine babesiosis, and now there are clinical evidences of possible vertical transmission too. Dogs of all ages can be affected with Babesia spp., but young puppies are more commonly affected. Two Babesia parasites were thought to occur in dogs; the relatively large intra-erythrocytic piroplasm referred to as Babesia canis and a smaller parasite, known predominantly as the cause of canine babesiosis in Asia, Babesia gibsoni. B. canis has been reclassified into three separate species (B. canis, B. rosi, B. vogeli) on the basis of immunity, serological testing, vector specificity and molecular phylogeny At least 4 genetically and clinically distinct small piroplasms affect dogs which include: Babesia gibsoni–originally described in India nearly a century ago and now occurring sporadically in other parts of the world including the Australia; Babesia conradae, a piroplasm that occasionally infects dogs in California; Theileria annae, a Babesia microti-like parasite that has so far been reported only in northwest Spain, transmitted by Ixodes hexagonus ; and a fourth small piroplasm, B. (=T.) equi has also been reported in dogs in Spain.³ Prevalence of Babesiosis The incidence of canine babesiosis vary considerably from one country to another depending on the distribution of the causative parasite and their specific vectors. Table below shows the data gathered during the Questionnaire-based survey on the distribution and incidence of canine babesiosis in countries of Western Europe.5 DIAGNOSIS, SYMPTOMS, AND TREATMENT Diagnosis. In the past, babesiosis was diagnosed by seeing the parasite on a blood smear. Other diagnostic tests are becoming more readily available, including FA (fluorescent antibody) staining of the organism and ELISA (enzyme-linked immunosorbent assay) tests. A PCR (polymerase chain reaction) test is also available and is commonly used to diagnose babesiosis. The PCR test has the advantage in that it can detect all four species of Babesia. Serologic or antibody titer testing in the diagnosis of babesiosis has limitations. A positive test result is dependent on an antibody response by the infected dog, which may take up to ten days to develop. Once a dog has developed antibodies to babesiosis, they may persist for years and this must be considered when performing follow-up tests.6 Symptoms. Dogs typically present with the acute, severe form of babesiosis, which is characterized by findings such as abnormally dark urine, fever, weakness, pale mucous membranes, depression, swollen lymph nodes, and an enlarged spleen. Potential complications: Bleeding problems, a severe type of anemia that leads to jaundice, organ damage, death.7 Treatment. The FDA approved treatment for babesiosis is imidocarb diproprionate. A combination therapy of quinine, azithromycin, atovaquone, and/or clindamycin is being researched and may become more common to treat dogs within the US or Canada in the future. Clindamycin, the treatment of choice for Babesia microti, the main Babesia species that infects humans, can also be used against Babesia in dogs. Clindamycin is a readily available antibiotic and is an excellent starting point for treatment in many dogs. Your veterinarian will discuss any alternative and adjunctive treatments with you.7 TRANSMISSION AND PREVENTION OF BABESIOSIS How is dog Babesia transmitted? Transmission. In most cases, Babesia organisms are spread to dogs through the bite of an infected tick but is not likely to be transmitted until a tick is attached for 36 hours. However, some studies suggest that infected dogs with open mouth sores can pass on the infection to other dogs through a bite, and infected pregnant females can transmit babesiosis to their unborn puppies. It can also be transmitted by the needle passage of infected blood, inadvertently in the case of blood transfusion or deliberately during experimental studies. Generic Life Cycle of Babesia spp.10 Generic life cycle of Babesia spp. Sporozoites (Sz) are injected into a vertebrate host blood system, during the blood meal of an infected tick. After invasion, Sz differentiate into trophozoites (T). Trophozoites undergo asexual division into two or four merozoites (M) in the infected red blood cells. Merozoites exit the red blood cells and invade new ones. Some groups of merozoites transform into gamonts or pregamotyces (G). The process of gamogony and sporogony takes place in the tick. Gamonts ingested by a tick feeding on an infected host differentiate in the gut into gametes (called ray bodies or Strahlenkorper – (Sk)) that fuse forming a diploid zygote (Z, gamogony). Via meiosis division, zygotes give rise to motile haploid kinetes. After haploid kinetes multiply by sporogony, they penetrate the tick haemolymph and organs. The final stage of the development occurs in the salivary glands (Sg), where differentiation and multiplication occur. Kinetes transform into sporozoites that infect the vertebrate host after vector development into a subsequent life stage – larvae to nymph, nymph to adult (transstadial transmission, Ts). In large Babesia spp. kinetes also invade the tick ovaries and eggs, and infective sporozoites are formed in the salivary glands of the next generation larvae. This process is called transovarial transmission (To). Adopted and reproducted from Schnittger et al. 9 How ticks spread disease11 Ticks transmit pathogens that cause disease through the process of feeding. Depending on the tick species and its stage of life, preparing to feed can take from 10 minutes to 2 hours. When the tick finds a feeding spot, it grasps the skin and cuts into the surface. The tick then inserts its feeding tube. Many species also secrete a cement-like substance that keeps them firmly attached during the meal. The feeding tube can have barbs which help keep the tick in place. Ticks also can secrete small amounts of saliva with anesthetic properties so that the animal or person can’t feel that the tick has attached itself. If the tick is in a sheltered spot, it can go unnoticed. A tick will suck the blood slowly for several days. If the host animal has a bloodborne infection, the tick will ingest the pathogens with the blood. Small amounts of saliva from
Thyroid Function in Animals

Sushant Sadotra Introduction: The thyroid is one of the endocrine glands in vertebrates. The thyroid gland has a bilobed structure located below the larynx and overlays the trachea in animals. In different animals, Anatomical variations of the thyroid are primarily seen in the isthmus connecting the gland’s two lobes. The size of the gland approximates 0.20% of body weight. However, the size may increase due to iodine deficiency, ingestion of goitrogenic toxins, tumors, and hyperactivity of the gland, or maybe reduced to fibrotic due to hyperthyroidism. Thyroid follicles are the thyroid gland’s functional units with a spherical structure composed of an inner core of the thyroglobulin-hormone complex, colloid. The colloid is surrounded by an outer monolayer of follicular cells and acts as the storage tank of thyroid hormone. The overall size of the follicles and the shape of their follicular cells may differ due to the functional activity of the thyroid gland. The dormant follicular cells are squamous-shaped compared to the tall columnar, highly active follicular cells. Other than colloid, the thyroid C-cells are interspersed between the follicles. The thyroid C-cells are the source of the hypocalcemic hormone calcitonin that is associated with calcium metabolism. The third type of tissue embedded in the thyroid gland is the parathyroid. The parathyroid is the source of the hypercalcemic hormone parathormone. Functions of the thyroid gland: The thyroid gland functions the same in all animals. There are four primary functions of the thyroid gland in animals; trapping the iodide, synthesis of thyroid hormones, storage, and release of hormones. All these activities of the thyroid gland are usually regulated by thyroid-stimulating hormone (TSH), a pituitary hormone. Hormonogenesis and release of thyroid hormone mainly have four stages: Trapping of Iodide: The follicular cells trap the circulating I– from the blood against the concentration gradient mediated by a sodium iodide symporter (NIS) protein present on the thyroid follicular cell membrane. A trapping enzyme catalyzes the trapping process via a mode of active transport catalyzed by an ATP-dependent Na+K+-ATPase. This trapping system’s high efficiency can concentrate most blood iodine in the thyroid gland. This process is stimulated by TSH and blocked by large amounts of I– or goitrogenic agents. (Figure 1) Synthesis of Thyroid Hormones: The trapping of I- is followed by its oxidation, catalyzed by peroxidase to form a highly active free radical I*. This reaction is also stimulated by TSH and inhibited by thyrotoxic agents (thiouracils or thioureas). At the follicular cell membrane-colloid interface, highly active I* binds to thyroglobulin, a thyroidal glycoprotein of a high molecular weight of 660 kDa. I* binds to thyroglobulin at its tyrosine moieties to form monoiodotyrosine (MIT) or a diiodotyrosine (DIT). After that, the iodinated phenyl groups of the tyrosine undergo oxidative condensation resulting in the synthesis of thyroid hormones. The thyroid gland produces two active hormones: 3,5,3’-triiodothyronine (T3) and 3,5,3′,5,-tetraiodothyronine (T4). T3 is formed by the oxidative condensation of an iodinated phenyl group of one DIT to an MIT group or of one DIT to another DIT to create T4. The inner deiodination product of the T4 is the inactive hormone is 3,3′,5’-triiodothyronine (rT3). Storage of hormones: Thyroid follicular cells synthesized thyroglobulin and localized it to the cell membrane for the iodination process. Iodinated thyroglobulin, also known as a colloid, is released and stored in the lumen of the follicle. Release of hormone: TSH stimulates the release process of hormones. TSH acts at the follicular cell membrane, the second site of action for TSH. Colloid from the lumen is taken up to the follicular membrane, where they are taken in as vesicles into the follicular cells by the process of endocytosis. Lysosomes merge with these vesicles to release lysosomal proteases that hydrolyze the colloid. Hydrolyses of colloid release their T3, T4, DIT, and MIT. Microsomal tyrosine deiodinases enzymatically degrade the released DIT and MIT, and their iodine is recycled within the follicular cell. A simple diffusion process releases the T4 and T3 into circulation. Out of the total hormone released from the gland, 90% is T4, and only 10% is T3. The phenyl group of T4 may also undergo some deiodination within the gland or in the peripheral tissues to form rT3. rT3 is an inactive form of the T3 hormone. Therefore it undergoes a degradation pathway. (Figure 1) The regulation of T3 and T4 secretion starts in the hypothalamus. The thyrotropin-releasing hormone secreted from the hypothalamus acts on the pituitary gland. This stimulates TSH secretion, which ultimately acts on the thyroid gland, producing and releasing thyroid hormones. The action and disorder of Thyroid Hormones: In humans and animals, thyroid hormones play a vital role in regulating metabolic and cellular mechanisms. The mode of action can be quick in minutes or prolonged to hours or longer. Thyroid hormones in normal levels work together with other hormones like insulin (beta cells of the pancreatic islets) and growth hormone (pituitary gland) to work on protein synthesis in different cellular processes. However, thyroid hormones can be catabolic in excess (hyperthyroidism), with increased protein breakdown and gluconeogenesis. Hyperthyroidism is more common in cats middle-aged to old cats than in dogs. However, thyroid carcinoma could be a cause when it occurs in dogs. Decreased levels of thyroid hormones (hypothyroidism) cause a slower metabolic rate in animals. This disorder is most likely seen in middle-aged (4-10 Years) dogs and mid to large-size dog breeds (Doberman pinscher, Golden retriever, etc.). Also, spayed female dogs have a higher hypothyroidism risk than unspayed ones. On the contrary, naturally occurring hypothyroidism is rare in cats. Reference: Kaneko, J. J. (2008). Clinical biochemistry of domestic animals. San Diego: Academic Press. Thanas C, Ziros PG, Chartoumpekis DV, Renaud CO, Sykiotis GP. The Keap1/Nrf2 Signaling Pathway in the Thyroid—2020 Update. Antioxidants. 2020; 9(11):1082. https://doi.org/10.3390/antiox9111082 Mark E. Peterson. The Thyroid Gland in Animals. Last full review/revision Jul 2019 | Content last modified Oct 2020. MSD MANUAL Veterinary Manual, https://www.msdvetmanual.com/endocrine-system/the-thyroid-gland/the-thyroid-gland-in-animals
Hyperthyroidism is not a risk factor for subclinical bacteriuria in cats: A prospective cohort study
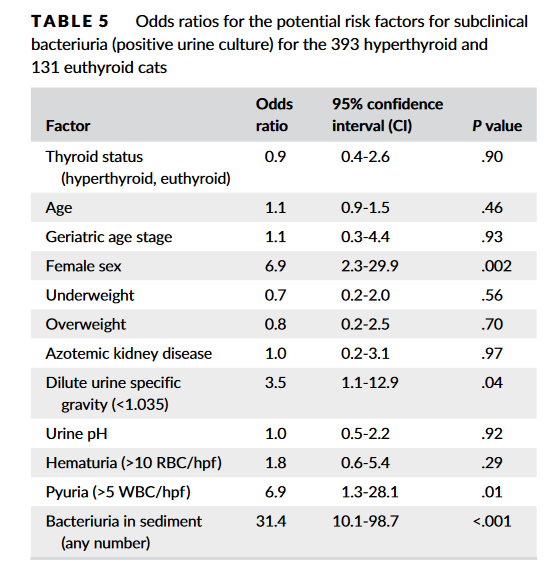
Source: https://doi.org/10.1111/jvim.15769 Subclinical bacteriuria is the presence of bacteria in urine with no clinical evidence of urinary tract infection (UTI). Some previous studies indicated that hyperthyroid cats are susceptible to UTIs (mostly subclinical) with prevalence rates of 12%-22%. As a result, many clinicians would recommend urine culture when evaluating hyperthyroid cats. To determine the true prevalence of subclinical bacteriuria in cats with hyperthyroidismIn, Eeterson M.E.’s group conducted a prospective cohort study. Both hyperthyroid and euthyroid cats had urine collected by cystocentesis for complete urinalysis and culture. Data pertaining to age, sex, body condition, and serum thyroxine and creatinine concentrations also were acquired. Hyperthyroid cats showed a low prevalence of subclinical bacteriuria (4.3%), which did not differ from that found in euthyroid cats (4.6%) in this study. In addition, only female sex was a significant risk factor. In conclusion, hyperthyroid cats are not at risk for subclinical bacteriuria.
Predicting Outcomes in Hyperthyroid Cats Treated with Radioiodine
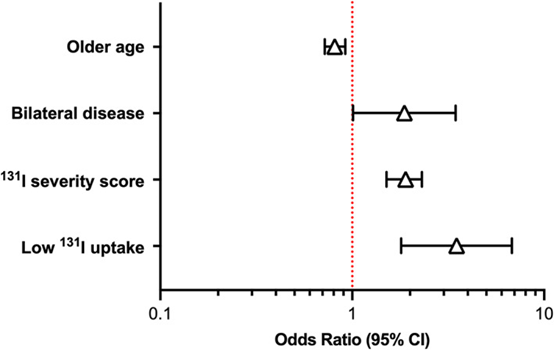
Source: J Vet Intern Med. 2022 Jan-Feb; 36(1): 49–58. doi: 10.1111/jvim.16319. Hyperthyroidism is a common disease in cats, and mostly afflicts cats middle-aged and older. It is caused by the overproduction of thyroid hormone by the thyroid glands. Radioiodine (131 I) is the treatment of choice to restore euthyroidism with a single dose of radiation without producing hypothyroidism for cats receiving the treatment. However, 30% to 50% of 131I‐treated cats develop iatrogenic hypothyroidism after treatment. Besides, 5% to 10% of hyperthyroid cats fail 131I treatment and remain persistently hyperthyroid. To identify pretreatment factors that may help predict persistent hyperthyroidism and iatrogenic hypothyroidism after treatment of cats using a novel 131I dosing algorithm. Peterson, ME and Rishniw, M conducted a study involving one thousand and four hundred hyperthyroid cats treated with 131I. Cats underwent an evaluation that included a complete physical examination, routine laboratory testing (CBC, serum biochemical profile, complete urinalysis), determination of serum thyroid hormone concentrations (total thyroxine [T4], triiodothyronine [T3], and thyroid‐stimulating hormone [TSH]), and qualitative and quantitative thyroid scintigraphy. Pretreatment predictors (clinical, laboratory, scintigraphic, 131I dose, 131I uptake measurements) of treatment failure or iatrogenic hypothyroidism were identified by multivariable logistic regression analysis. In conclusion, Age, sex, serum TSH concentration, bilateral and homogeneous 99mTc‐pertechnetate uptake on scintigraphy, severity score, and percent 131I uptake are all factors that might help predict outcome of 131I treatment in hyperthyroid cats. For detail information please check the original paper: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8783366/
Individualized I-131 Dosing for Feline Hyperthyroidism Treatment
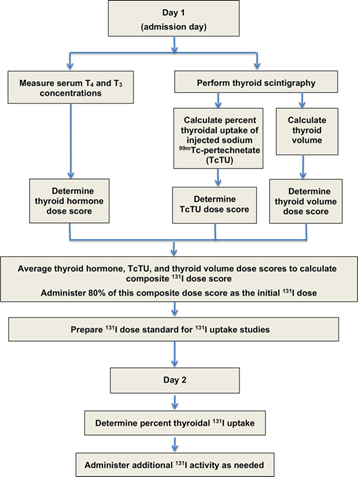
Table of Contents 1. Introduction 1.1 Overview of Feline Hyperthyroidism Feline hyperthyroidism is the most common endocrine disorder affecting middle-aged and geriatric cats, driven overwhelmingly by autonomous thyroid adenomas or adenomatous hyperplasia. More than 97 percent of cases result from benign, functional proliferation of thyroid tissue that produces excessive amounts of thyroxine (T4) and triiodothyronine (T3) (Peterson, 2013; Broussard et al., 1995). The resulting hypermetabolic state manifests across multiple organ systems. Typical clinical signs include: Progressive weight loss, despite normal or increased appetite Polyphagia, polydipsia, and polyuria Episodic vomiting or diarrhea A dull or unkempt hair coat Tachycardia and a palpable thyroid nodule in many cases These signs often begin subtly, then intensify as thyroid hormone excess accelerates metabolic turnover and causes secondary strain on cardiovascular, renal, and gastrointestinal systems. 1.2 Limitations of Traditional Radioiodine (I-131) Dosing Radioiodine (I-131) therapy is widely regarded as the treatment of choice for feline hyperthyroidism (Peterson, 2013; Mooney, 2001; Feldman & Nelson, 2015). I-131 concentrates selectively in hyperfunctional thyroid tissue, where emitted beta particles induce cytotoxicity and subsequent glandular fibrosis. Traditional fixed-dose approaches, typically ranging from 3–5 mCi, have historically produced good cure rates Peterson, 2013; Williams et al., 2010; Peterson & Broome, 2015). However, these protocols are increasingly recognized as imprecise, with substantial rates of treatment-related complications: Iatrogenic Hypothyroidism (IH).Fixed-dose regimens often exceed the minimal therapeutic requirement, exposing normal thyroid remnants to unnecessary radiation. Reported IH rates vary widely—from 30 to 80 percent—and represent a major concern in post-treatment management. IH-associated azotemia carries significant prognostic implications. Cats that become hypothyroid and azotemic after treatment have significantly shorter survival times than cats that remain euthyroid or non-azotemic. This underscores the clinical importance of avoiding overtreatment. 1.3 Evidence Supporting Individualized Radioiodine Dosing To mitigate these risks, Peterson and Rishniw (2021) developed a sophisticated, feline-specific dosing algorithm designed to deliver the lowest effective I-131 dose required to achieve euthyroidism while minimizing the likelihood of iatrogenic hypothyroidism and azotemia. Drawing on data from 1,400 hyperthyroid cats, their study established several crucial findings: Median total dose: 1.9 mCi (range 1.0–10.6 mCi)• Considerably lower than historical fixed-dose practices Cure (euthyroid) rate: 74.8 percent, comparable to traditional outcomes Significantly lower complication rates:• 4.1 percent overt hypothyroidism• 17.1 percent subclinical hypothyroidism• Combined rate (~21%) markedly lower than many fixed-dose protocols These outcomes demonstrate that tailored dosing not only achieves therapeutic efficacy but also reduces the risk burden associated with excessive radiation exposure. The Two-Day Algorithmic Protocol The algorithm employs a structured, multiparametric approach based on objective measures of disease severity and biological iodine-handling capacity. Day 1: Initial Composite Dose (80 percent administered) A composite dose score is calculated by integrating three major disease indicators: Serum T4 and T3 concentrations Thyroid tumor volume, measured using thyroid scintigraphy Technetium uptake (TcTU), a marker of functional thyroid activity Only 80 percent of this calculated composite dose is administered initially to avoid overtreatment. Day 2: Uptake-Based Dose Adjustment Approximately 24 hours later, the thyroidal I-131 uptake is measured to determine how effectively the gland concentrates radioiodine. A supplemental dose is then administered as needed. In the study, 1,380 out of 1,400 cats required additional I-131 on Day 2, highlighting the essential role of uptake-based adjustment and the variability in individual glandular kinetics. This two-step method mirrors the logic of precision dosing used in pharmaceutical sciences:deliver enough activity to neutralize the hyperfunctioning tissue, but not so much that normal thyroid function is extinguished or renal sequelae are exacerbated. 2. Radioiodine Pharmacology The therapeutic use of radioiodine (131I) in feline hyperthyroidism rests on a sophisticated interplay between thyroid physiology, nuclear physics, and disciplined radiation-safety practices. The following section synthesizes the core pharmacologic principles, uptake kinetics, veterinary dosimetry, and regulatory safety frameworks that underpin this therapy. 2.1 Mechanism of 131I Radioiodine (131I) exploits the thyroid gland’s unique ability to concentrate iodine for hormone synthesis. Targeting mechanism.The follicular cells of the thyroid actively transport iodine from the bloodstream using the sodium–iodide symporter (NIS). Because the NIS cannot distinguish between stable iodine and 131I, hyperfunctional thyroid tissue accumulates radioiodine to levels that far exceed blood concentrations, often by a factor of 500-fold. In hyperthyroid cats, adenomatous tissue is especially efficient at concentrating 131I. Destructive mechanism.Once incorporated into the gland, 131I decays as a dual-emitter. Its therapeutic activity derives largely from the emission of high-energy beta (β–) particles, which: have a short path length (typically 0.5–2 mm, mean 0.8 mm), generate highly localized cell injury, induce pyknosis, necrosis, and progressive fibrosis over subsequent weeks. This short-range cytotoxicity spares adjacent structures—including the parathyroid glands—substantially reducing the risk of hypoparathyroidism. Selective destruction.In hyperthyroid cats, normal thyroid tissue is usually suppressed by low endogenous TSH levels and therefore takes up minimal 131I. This endogenous suppression optimizes therapeutic selectivity by focusing the radiation burden on the diseased tissue. 2.2 Thyroid Uptake Kinetics Biological and effective half-life.While the physical half-life of ^131I is 8.04 days, the effective half-life in hyperthyroid cats is shorter—approximately 2.3 to 2.54 days—reflecting both physical decay and biological elimination. Renal clearance.Elimination of circulating 131I occurs primarily via renal excretion. Cats with renal disease may retain 131I longer, increasing total radiation burden and necessitating more cautious monitoring. Role of uptake measurement.In individualized radioiodine dosing protocols, 24-hour thyroidal 131I uptake is measured to refine and optimize the total therapeutic dose. This uptake assessment serves as a physiologic indicator of how efficiently the thyroid tissue concentrates radioiodine, allowing clinicians to adjust the administered activity accordingly. Low uptake values signal reduced radioiodine concentration and therefore pose a risk of undertreatment, potentially leading to persistent hyperthyroidism. Conversely, high uptake values increase the likelihood of excessive radiation delivery, elevating the risk of iatrogenic hypothyroidism. As such, measuring thyroidal 131I uptake is pivotal for balancing therapeutic efficacy with preservation of normal endocrine function, and it represents a central component of individualized dosing algorithms. 2.3 Veterinary Dosimetry Considerations Modern veterinary dosimetry emphasizes delivering the lowest effective dose to achieve euthyroidism while minimizing complications such as hypothyroidism and azotemia. The individualized 2-day dosage algorithm used by Peterson and Rishniw (2021)
Lameness, Generalised Myopathy and Myalgia in an Adult Cat with Toxoplasmosis- Abstract Butts DR, Langley-Hobbs SJ.

Source: JFMS Open Rep. 2020 Mar 13;6(1):2055116920909668. doi: 10.1177/2055116920909668. A 2-year-old female neutered domestic shorthair cat presented with an 18-month history of intermittent lameness on all four limbs. The cat was markedly lame on all four limbs. Physical examination detected pain on palpation of the calcaneus bone and Achilles tendon bilaterally, and general resentment to handling. Investigations revealed an elevated creatine kinase, a positive Toxoplasma gondii IgG titre, toxic neutrophilic inflammation within the Achilles tendon bursae, electromyography and nerve conduction velocity studies consistent with a diffuse muscular disease, and histopathology of the muscle consistent with a chronic and diffuse myopathy. Arthrocentesis samples and an antinuclear antibodies titre were normal. Prior treatment with meloxicam had been ineffective. A 6-week course of clindamycin was prescribed; an improvement was seen within 3 days and clinical resolution at 3 months. The cat remained clinically normal after 20 months. This report suggests toxoplasmosis should be considered as a differential diagnosis in cats with myopathies or lameness in the absence of other causes. Figure 1 Toe-walking on the left forelimb with hunched posture. (b) Weightbearing on the dorsal aspect of the left carpus. (c) Sitting back on the hindlimbs and non-weightbearing on the forelimbs Figure 2 Neutrophil containing a duck egg blue cytoplasmic inclusion (far left) seen on cytology of Achilles tendon bursal fluid (suspected to be a lupus cell or Döhle body)
Generalized Alopecia with Vasculitis-Like Changes in a Dog with Babesiosis- Abstract Tasaki Y, Miura N, Iyori K, Nishifuji K, Endo Y, Momoi Y. J

Source: Vet Med Sci. 2013 Oct;75(10):1367-9. doi: 10.1292/jvms.12-0482. A 12-year-old, intact female Satsuma dog was referred to the Kagoshima University Veterinary Teaching Hospital due to skin lesions. Clinical symptoms include erythema, crusts and desquamation on the truck, papules and erosions in the pinnae, and multiple areas of skin necrosis on the right forelimb. Treatment with systemic antibiotics and prednisolone did not improve the observed symptoms. The dog also had progressive anemia. Babesia gibsoni was detected in the blood via PCR during its second visit, and the dog was treated with antiprotozoal agents. Though the cutaneous lesions and anemia improved, skin lesions relapsed after the treatment was discontinued. Histopathological examination of skin biopsies revealed findings suggestive of early leukocytoclastic vasculitis or ischemic vasculopathy… Fig. 1. A–D: Appearance of the dog on initial presentation. A: Alopecia, scales and desquamation in the lumbar area. B: Alopecia and erythema on the trunk. C: Erosion and crusts in the pinnae. D: Cutaneous necrosis on the right forelimb. E, F: Appearance during remission after approximately 2 months of antiprotozoal therapy. E: Alopecia and other skin lesions on the trunk are improved, and the hair color changed from light brown to dark brown. F: Erosion and crusts disappear in the pinnae. Fig. 2. Histopathological sections of affected skin. A: Lower magnification showing perivascular infiltration of inflammatory cells in the middle portion of dermis. Edema and intense extravasation are seen in the superficial dermis. B: Higher magnification of A showing infiltration of neutrophils into the vessel walls and perivascular area, and fibrin deposition adjacent to the blood vessels.
Cortisol: A Short Review
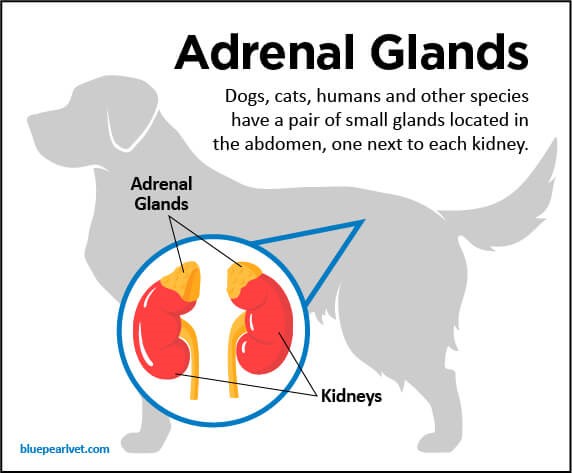
Maigan Espinili Maruquin The well- being of animal can be monitored from stress levels, which is related to the hypothalamic-pituitary-adrenocortical (HPA) axis activity (Möstl and Palme 2002, Salaberger, Millard et al. 2016). Elevation of glucocorticoid concentrations are observed in stressful situations (Salaberger, Millard et al. 2016). https://bluepearlvet.com/medical-articles-for-pet-owners/addisons-disease-in-dogs/ Fig. 01. Location of Adrenal glands which produces glucocorticoids Cortisol is known to play an important role in the interconnected responses on physiological, behavioral, and developmental functions (Bennett and Hayssen 2010). As an adrenal glucocorticoid, acute stress response result to rapid release of glucose from energy stores, suppresses inflammation, and promotes immune cell proliferation (Sapolsky, Romero et al. 2000, Charmandari, Tsigos et al. 2005, Mack and Fokidis 2017). Although measuring cortisol used to require significant disruption in behavior, different non- invasive sample collection methods for cortisol is now being used (Bennett and Hayssen 2010). Cortisol Concentration at Different Tissues In humans, salivary cortisol concentration for measurement is popular due to its straightforwardness and minimal invasive effect, including the fact that the storage is easy (Chen, Cintrón et al. 1992, Wenger-Riggenbach, Boretti et al. 2010). For healthy dogs, cortisol is unbound and passively diffuses from blood to saliva (Kirschbaum, C., et al, 1992) (Vincent and Michell 1992, Cobb, Iskandarani et al. 2016). Within 5 minutes, concentration of free cortisol in saliva and plasma sets at an equilibrium (Tunn, Möllmann et al. 1992, Wenger-Riggenbach, Boretti et al. 2010). Although blood and saliva can provide immediate view of cortisol concentrations, blood collection can be stressful, causing elevated concentrations. On the other hand, saliva absorption materials cause inconsistent results (Dreschel and Granger 2009, Bennett and Hayssen 2010). Cortisol concentrations can be measured for a short time in urine and fecal samples (Bennett and Hayssen 2010). In urine, maximum concentration can be reached at approximately 3 hours (Rooney, Gaines et al. 2007, Bennett and Hayssen 2010) and longer in fecal samples (Bennett and Hayssen 2010). Aside from daily fluctuation of cortisol concentrations in saliva, blood, and urine (van Vonderen, Kooistra et al. 1998), it can also be influenced by any stress of the animal (Kobelt, Hemsworth et al. 2003, Mack and Fokidis 2017). A lot of keratinized tissues contain glucocorticoids (Mack and Fokidis 2017). Concentration in the hair provides a long- term information on glucocorticoid production compared to the concentrations during sample collection (Ouschan, Kuchar et al. 2013). However, based on the effects of hair sampling, analysis of long-term cortisol secretion may be complicated (Mack and Fokidis 2017). Hair may also serve as cortisol storage area, however, validation for every species may be required due to difference in cortisol rhythms, secretions and stress response (Bennett and Hayssen 2010). On the other hand, a study was conducted using dog nails to assess cortisol concentration, wherein nail accumulates cortisol passively from the bloodstream (Mack and Fokidis 2017). Hyperadrenocorticism and Hypoadrenocorticism The chronic overexposure to glucocorticoids like cortisol can result to a complex physical and biochemical changes, referred to as hyperadrenocorticism (HAC) (Ouschan, Kuchar et al. 2013). Clinical signs of an affected dog show polyuria, polydipsia, polyphagia, pot-bellied appearance and typical skin and hair changes (Ouschan, Kuchar et al. 2013) (Feldman EC & Nelson RW, 2004). A tumor in the pituitary gland is usually the cause of this disease, wherein it secretes adrenocorticotrophic hormone (ACTH) and stimulates adrenal glands, resulting to glucocorticoids production (Ouschan, Kuchar et al. 2013). For humans, diagnosis of hypercortisolism and hypocortisolism through the late-night and morning salivary cortisol concentrations is the established screening test (Viardot, Huber et al. 2005, Nieman, Biller et al. 2008, Restituto, Galofré et al. 2008, Wenger-Riggenbach, Boretti et al. 2010). On the other hand, glucocorticoid deficiency is termed to as hypoadrenocorticism (Peterson, Kintzer et al. 1996), wherein, primary adrenal gland failure is the cause of most cases in dogs (Peterson, Kintzer et al. 1996, Gold, Langlois et al. 2016) (Scott-Moncrieff JC, 2010). Due to general and non- specific clinicopathologic signs, it is confused with primary gastrointestinal, renal, or cardiovascular disease. On-time and accurate diagnosis is important because it is a life-threatening disease if it goes without appropriate treatment (Gold, Langlois et al. 2016). References: Addison’s Disease in Dogs Scott-Moncrieff JC. Hypoadrenocorticism. In: Ettinger SJ, Feldman EC, eds. Textbook of Veterinary Internal Medicine, 7th ed. volume 2. St. Louis, MO: Saunders; 2010:1847–1857. Feldman EC, Nelson RW. Canine hyperadrenocorticism (Cushing′s syndrome). In: Canine and Feline Endocrinology and Reproduction. 3rd edn. St Louis: Saunders, 2004; 252–357. Kirschbaum C, Read GF, Hellhammer D. Assessment of hormones and drugs in saliva in biobehavioral research. Seattle, WA: Hogrefe & Huber; 1992. p. 19–32. Bennett, A. and V. Hayssen (2010). “Measuring cortisol in hair and saliva from dogs: coat color and pigment differences.” Domestic Animal Endocrinology 39(3): 171-180. Charmandari, E., C. Tsigos and G. Chrousos (2005). “ENDOCRINOLOGY OF THE STRESS RESPONSE.” Annual Review of Physiology 67(1): 259-284. Chen, Y. M., N. M. Cintrón and P. A. Whitson (1992). “Long-term storage of salivary cortisol samples at room temperature.” Clin Chem 38(2): 304. Cobb, M. L., K. Iskandarani, V. M. Chinchilli and N. A. Dreschel (2016). “A systematic review and meta-analysis of salivary cortisol measurement in domestic canines.” Domestic Animal Endocrinology 57: 31-42. Dreschel, N. A. and D. A. Granger (2009). “Methods of collection for salivary cortisol measurement in dogs.” Horm Behav 55(1): 163-168. Gold, A. J., D. K. Langlois and K. R. Refsal (2016). “Evaluation of Basal Serum or Plasma Cortisol Concentrations for the Diagnosis of Hypoadrenocorticism in Dogs.” Journal of Veterinary Internal Medicine 30(6): 1798-1805. Kobelt, A. J., P. H. Hemsworth, J. L. Barnett and K. L. Butler (2003). “Sources of sampling variation in saliva cortisol in dogs.” Res Vet Sci 75(2): 157-161. Mack, Z. and H. B. Fokidis (2017). “A novel method for assessing chronic cortisol concentrations in dogs using the nail as a source.” Domestic Animal Endocrinology 59: 53-57. Möstl, E. and R. Palme (2002). “Hormones as indicators of stress.” Domestic Animal Endocrinology 23(1): 67-74. Nieman, L. K., B. M. Biller, J. W. Findling, J. Newell-Price, M. O. Savage, P. M. Stewart and V. M.
