Breed-related disease: Bichon Frise

The Bichon Frise is often depicted as a French dog. Although the Bichon breed type are originally Spanish, used as sailing dogs, also as herding dogs sometimes, the French developed them into a gentle lap-dog variety. The Bichon type arose from the water dogs, and is descended from the poodle-type dogs and either the Barbet or one of the water spaniel class of breeds. Modern Bichons have developed into four categories: the Bichon Frise or Tenerife, the Maltese, the Bolognese, and the Havanese. These are often treated as separate breeds. A good-size Bichon will stand a shade under a foot tall at the shoulder. The breed’s glory is a white hypoallergenic coat, plush and velvety to the touch, featuring rounded head hair that sets off the large, dark eyes and black leathers of the nose and lips. With its happy-go-lucky attitude, the playful, vivacious, and bouncy Bichon dog delights everyone. It is good with kids and amicable towards pets, other dogs, and strangers. This affectionate, responsive, and sensitive dog also loves to play and be cuddled, but when it is left alone, it may bark excessively. The Bichon dog breed, with a lifespan of about 12 to 15 years, is prone to some serious health problems like: Heart Disease: Bichons are prone to multiple types of heart disease, which can occur both early and later in life. Liver Problems: Your Bichon is more likely than other dogs to have a liver disorder called portosystemic shunt (PSS). Some of the blood supply that should go to the liver goes around it instead, depriving the liver of the blood flow it needs to grow and function properly. If your friend has PSS, his liver cannot remove toxins from his bloodstream effectively. Hip Dysplasia Hip dysplasia is a hereditary condition that prevents the thigh bone from adjusting perfectly to the hip joint. Hip dysplasia is common among Bichon Frise, but it does not affect them all. The dog usually has symptoms of pain and lameness. However, hip dysplasia does not always cause discomfort in the Bichon Frise, but it can develop into arthritis as your dog ages. Incontinence Incontinence can affect your Bichon Frise at any age. If your dog has been previously housetrained, it is important to remember that loss of bladder or bowel control is a physical problem, not a behavioral one. Incontinence is most commonly found in older Bichon Frises, especially females. Source: https://en.wikipedia.org/wiki/Bichon_Frise Photo credit: https://en.wikipedia.org/wiki/Bichon_Frise
Breed-related disease: Japanese Bobtail

The Japanese Bobtail is a breed of domestic cat with an unusual bobtail more closely resembling the tail of a rabbit than that of other cats. The variety is native to Japan and Southeast Asia, though it is now found throughout the world. The breed has been known in Japan for centuries, and it frequently appears in traditional folklore and art. Japanese bobtails have two coat types: long and short. The coat can be solid, bi-color, calico, or tabby, but this breed is most commonly white with colored spots, or what some call the van pattern. Both long and short coats are silky smooth, easy to groom, and low-shedding. However, although Japanese bobtails usually shed less than other breeds, they do have shedding seasons in the spring and fall and are not considered hypoallergenic. The Japanese Bobtail is active and intelligent. It’s not unusual to find him splashing his paw in water, carrying toys around, or playing fetch. He is highly curious and loves to explore. Japanese Bobtails are talkative, communicating with a wide range of chirps and meows. Their voices are described as almost songlike. These are outgoing cats who get along well with children and other pets, including dogs, and adjust to travel with ease. They love people and are often seen riding on a shoulder so they can supervise everything going on. We know that because you care so much about your cat, you want to take great care of her. That is why we have summarized the health concerns we will be discussing with you over the life of your Japanese bobtail. Dental Disease: Dental disease is one of the most common chronic problems in pets who don’t have their teeth brushed regularly. Unfortunately, most cats don’t take very good care of their own teeth, and this probably includes your Japanese bobtail. Without extra help and care from you, your cat is likely to develop potentially serious dental problems. Dental disease starts with food residue, which hardens into tartar that builds up on the visible parts of the teeth, and eventually leads to infection of the gums and tooth roots. Protecting your cat against dental disease from the start by removing food residue regularly may help prevent or delay the need for advanced treatment of dental disease. Heart Disease: Cardiomyopathy is the medical term for heart muscle disease, either a primary inherited condition or secondary to other diseases that damage the heart. The most common form, called hypertrophic cardiomyopathy, or HCM, is a thickening of the heart muscle often caused by an overactive thyroid gland. Another example is dilated cardiomyopathy, or DCM, which can be caused by a dietary deficiency of the amino acid taurine. While DCM was a big problem in the past, all major cat food producers now add taurine to cat food, so DCM is rarely seen in cats with high-quality diets today. FLUTD: When your cat urinates outside the litter box, you may be annoyed or furious, especially if your best pair of shoes was the location chosen for the act. But don’t get mad too quickly—in the majority of cases, cats who urinate around the house are sending signals for help. Although true urinary incontinence, the inability to control the bladder muscles, is rare in cats and is usually due to improper nerve function from a spinal defect, most of the time, a cat that is urinating in “naughty” locations is having a problem and is trying to get you to notice. What was once considered to be one urinary syndrome has turned out to be several over years of research, but current terminology gathers these different diseases together under the label of Feline Lower Urinary Tract Diseases, or FLUTD. Renal Failure: Renal failure refers to the inability of the kidneys to properly perform their functions of cleansing waste from the blood and regulating hydration. Kidney disease is extremely common in older cats, but is usually due to exposure to toxins or genetic causes in young cats. Even very young kittens can have renal failure if they have inherited kidney defects, so we recommend screening for kidney problems early, before any anesthesia or surgery, and then regularly throughout life. Severe renal failure is a progressive, fatal disease, but special diets and medications can help cats with kidney disease live longer, fuller lives. Source: https://www.cbvetclinic.com/client-resources/breed-info/japanese-bobtail-longhair/ https://www.cat-lovers-only.com/japanese-bobtail.html Photo crédit: https://www.petfinder.com/cat-breeds/japanese-bobtail/
Generalized Alopecia with Vasculitis-Like Changes in a Dog with Babesiosis- Abstract Tasaki Y, Miura N, Iyori K, Nishifuji K, Endo Y, Momoi Y. J

Source: Vet Med Sci. 2013 Oct;75(10):1367-9. doi: 10.1292/jvms.12-0482. A 12-year-old, intact female Satsuma dog was referred to the Kagoshima University Veterinary Teaching Hospital due to skin lesions. Clinical symptoms include erythema, crusts and desquamation on the truck, papules and erosions in the pinnae, and multiple areas of skin necrosis on the right forelimb. Treatment with systemic antibiotics and prednisolone did not improve the observed symptoms. The dog also had progressive anemia. Babesia gibsoni was detected in the blood via PCR during its second visit, and the dog was treated with antiprotozoal agents. Though the cutaneous lesions and anemia improved, skin lesions relapsed after the treatment was discontinued. Histopathological examination of skin biopsies revealed findings suggestive of early leukocytoclastic vasculitis or ischemic vasculopathy… Fig. 1. A–D: Appearance of the dog on initial presentation. A: Alopecia, scales and desquamation in the lumbar area. B: Alopecia and erythema on the trunk. C: Erosion and crusts in the pinnae. D: Cutaneous necrosis on the right forelimb. E, F: Appearance during remission after approximately 2 months of antiprotozoal therapy. E: Alopecia and other skin lesions on the trunk are improved, and the hair color changed from light brown to dark brown. F: Erosion and crusts disappear in the pinnae. Fig. 2. Histopathological sections of affected skin. A: Lower magnification showing perivascular infiltration of inflammatory cells in the middle portion of dermis. Edema and intense extravasation are seen in the superficial dermis. B: Higher magnification of A showing infiltration of neutrophils into the vessel walls and perivascular area, and fibrin deposition adjacent to the blood vessels.
Cortisol: A Short Review
Maigan Espinili Maruquin The well- being of animal can be monitored from stress levels, which is related to the hypothalamic-pituitary-adrenocortical (HPA) axis activity (Möstl and Palme 2002, Salaberger, Millard et al. 2016). Elevation of glucocorticoid concentrations are observed in stressful situations (Salaberger, Millard et al. 2016). https://bluepearlvet.com/medical-articles-for-pet-owners/addisons-disease-in-dogs/ Fig. 01. Location of Adrenal glands which produces glucocorticoids Cortisol is known to play an important role in the interconnected responses on physiological, behavioral, and developmental functions (Bennett and Hayssen 2010). As an adrenal glucocorticoid, acute stress response result to rapid release of glucose from energy stores, suppresses inflammation, and promotes immune cell proliferation (Sapolsky, Romero et al. 2000, Charmandari, Tsigos et al. 2005, Mack and Fokidis 2017). Although measuring cortisol used to require significant disruption in behavior, different non- invasive sample collection methods for cortisol is now being used (Bennett and Hayssen 2010). Cortisol Concentration at Different Tissues In humans, salivary cortisol concentration for measurement is popular due to its straightforwardness and minimal invasive effect, including the fact that the storage is easy (Chen, Cintrón et al. 1992, Wenger-Riggenbach, Boretti et al. 2010). For healthy dogs, cortisol is unbound and passively diffuses from blood to saliva (Kirschbaum, C., et al, 1992) (Vincent and Michell 1992, Cobb, Iskandarani et al. 2016). Within 5 minutes, concentration of free cortisol in saliva and plasma sets at an equilibrium (Tunn, Möllmann et al. 1992, Wenger-Riggenbach, Boretti et al. 2010). Although blood and saliva can provide immediate view of cortisol concentrations, blood collection can be stressful, causing elevated concentrations. On the other hand, saliva absorption materials cause inconsistent results (Dreschel and Granger 2009, Bennett and Hayssen 2010). Cortisol concentrations can be measured for a short time in urine and fecal samples (Bennett and Hayssen 2010). In urine, maximum concentration can be reached at approximately 3 hours (Rooney, Gaines et al. 2007, Bennett and Hayssen 2010) and longer in fecal samples (Bennett and Hayssen 2010). Aside from daily fluctuation of cortisol concentrations in saliva, blood, and urine (van Vonderen, Kooistra et al. 1998), it can also be influenced by any stress of the animal (Kobelt, Hemsworth et al. 2003, Mack and Fokidis 2017). A lot of keratinized tissues contain glucocorticoids (Mack and Fokidis 2017). Concentration in the hair provides a long- term information on glucocorticoid production compared to the concentrations during sample collection (Ouschan, Kuchar et al. 2013). However, based on the effects of hair sampling, analysis of long-term cortisol secretion may be complicated (Mack and Fokidis 2017). Hair may also serve as cortisol storage area, however, validation for every species may be required due to difference in cortisol rhythms, secretions and stress response (Bennett and Hayssen 2010). On the other hand, a study was conducted using dog nails to assess cortisol concentration, wherein nail accumulates cortisol passively from the bloodstream (Mack and Fokidis 2017). Hyperadrenocorticism and Hypoadrenocorticism The chronic overexposure to glucocorticoids like cortisol can result to a complex physical and biochemical changes, referred to as hyperadrenocorticism (HAC) (Ouschan, Kuchar et al. 2013). Clinical signs of an affected dog show polyuria, polydipsia, polyphagia, pot-bellied appearance and typical skin and hair changes (Ouschan, Kuchar et al. 2013) (Feldman EC & Nelson RW, 2004). A tumor in the pituitary gland is usually the cause of this disease, wherein it secretes adrenocorticotrophic hormone (ACTH) and stimulates adrenal glands, resulting to glucocorticoids production (Ouschan, Kuchar et al. 2013). For humans, diagnosis of hypercortisolism and hypocortisolism through the late-night and morning salivary cortisol concentrations is the established screening test (Viardot, Huber et al. 2005, Nieman, Biller et al. 2008, Restituto, Galofré et al. 2008, Wenger-Riggenbach, Boretti et al. 2010). On the other hand, glucocorticoid deficiency is termed to as hypoadrenocorticism (Peterson, Kintzer et al. 1996), wherein, primary adrenal gland failure is the cause of most cases in dogs (Peterson, Kintzer et al. 1996, Gold, Langlois et al. 2016) (Scott-Moncrieff JC, 2010). Due to general and non- specific clinicopathologic signs, it is confused with primary gastrointestinal, renal, or cardiovascular disease. On-time and accurate diagnosis is important because it is a life-threatening disease if it goes without appropriate treatment (Gold, Langlois et al. 2016). References: Addison’s Disease in Dogs Scott-Moncrieff JC. Hypoadrenocorticism. In: Ettinger SJ, Feldman EC, eds. Textbook of Veterinary Internal Medicine, 7th ed. volume 2. St. Louis, MO: Saunders; 2010:1847–1857. Feldman EC, Nelson RW. Canine hyperadrenocorticism (Cushing′s syndrome). In: Canine and Feline Endocrinology and Reproduction. 3rd edn. St Louis: Saunders, 2004; 252–357. Kirschbaum C, Read GF, Hellhammer D. Assessment of hormones and drugs in saliva in biobehavioral research. Seattle, WA: Hogrefe & Huber; 1992. p. 19–32. Bennett, A. and V. Hayssen (2010). “Measuring cortisol in hair and saliva from dogs: coat color and pigment differences.” Domestic Animal Endocrinology 39(3): 171-180. Charmandari, E., C. Tsigos and G. Chrousos (2005). “ENDOCRINOLOGY OF THE STRESS RESPONSE.” Annual Review of Physiology 67(1): 259-284. Chen, Y. M., N. M. Cintrón and P. A. Whitson (1992). “Long-term storage of salivary cortisol samples at room temperature.” Clin Chem 38(2): 304. Cobb, M. L., K. Iskandarani, V. M. Chinchilli and N. A. Dreschel (2016). “A systematic review and meta-analysis of salivary cortisol measurement in domestic canines.” Domestic Animal Endocrinology 57: 31-42. Dreschel, N. A. and D. A. Granger (2009). “Methods of collection for salivary cortisol measurement in dogs.” Horm Behav 55(1): 163-168. Gold, A. J., D. K. Langlois and K. R. Refsal (2016). “Evaluation of Basal Serum or Plasma Cortisol Concentrations for the Diagnosis of Hypoadrenocorticism in Dogs.” Journal of Veterinary Internal Medicine 30(6): 1798-1805. Kobelt, A. J., P. H. Hemsworth, J. L. Barnett and K. L. Butler (2003). “Sources of sampling variation in saliva cortisol in dogs.” Res Vet Sci 75(2): 157-161. Mack, Z. and H. B. Fokidis (2017). “A novel method for assessing chronic cortisol concentrations in dogs using the nail as a source.” Domestic Animal Endocrinology 59: 53-57. Möstl, E. and R. Palme (2002). “Hormones as indicators of stress.” Domestic Animal Endocrinology 23(1): 67-74. Nieman, L. K., B. M. Biller, J. W. Findling, J. Newell-Price, M. O. Savage, P. M. Stewart and V. M.
Breed-related disease: Airedale Terrier

John K. Rosembert The Airedale Terrier also called Bingley Terrier and Waterside Terrier, is a dog breed of the terrier type that originated in the valley (dale) of the River Aire, in the West Riding of Yorkshire, England. It is traditionally called the “King of Terriers” because it is the largest of the terrier breeds. The Airedale was bred from the Old English Black and Tan Terrier (now known as the Welsh Terrier), the Otterhound and probably some other Terrier breeds, and has contributed to other dog breeds, such as the Yorkshire Terrier. Originally bred to serve as a versatile hunting and all around working farm dog, in Britain this breed has also been used as a war dog, guide dog and police dog. In the United States, this breed has been used to hunt big game, upland birds, and water fowl, and serve in many other working capacities. The Airedale Terrier is known as the “king of terriers” partly for his size. They range in height about 23 inches and in weight from 45 pounds for a small female, to 70 pounds for a large male (20 to 32 kilograms).the breed has a classic terrier head with virtually no stop (forehead), v-shaped ears tipped over and a straight back with an erect docked tail. The outline is quite square and these dogs are sturdy. Coloring for the Airedale is black and tan, with a classic terrier coat of dense, harsh hair with a softer undercoat. A grown out coat will look almost curly. The coat and color stay sharpest with hand stripping of the dead hair. Pet Airedales that are clipped may appear gray and tan. This protective and lively companion is one of the most versatile terriers. The playful, adventurous, and bold Airedale is intelligent, and yet headstrong and stubborn at times. Though some dogs are dominating, most of them are responsive to the wishes of the owner and are reliable. As long as the Airedale is provided with daily physical and mental exercise, it is a well-behaved house dog. It likes to be a leader and dislikes being challenged by other dogs. Smaller dogs and terriers, however, get along well. We know you care so much for your dog welfare, below we summarize some of the most common problem of the terrier dog Eye Problems Not many things have as dramatic an impact on your dog’s quality of life as the proper functioning of his eyes. Unfortunately, Airedale Terriers can inherit or develop a number of different eye conditions, some of which may cause blindness if not treated right away, and most of which can be extremely painful! We will evaluate his eyes at every examination to look for any signs of concern. Hip dysplasia Hip dysplasia is one of the most commonly found osteopathic conditions in pedigree dog breeds, and the Airedale is one of the breeds that is known to be affected by it to some degree. Hip dysplasia has a genetic element to it, and is caused by a malformation of the hip joint in development, which usually manifests in dogs before they reach the age of two years old. Dermatitis Airedales can be prone to a range of skin conditions, particularly dermatitis, which is common across all of the terrier breeds. The coat and skin of Airedales should be checked over regularly, as problems often go unnoticed due to the density of their coats. Acral lick granulomas may develop if sore spots and itching lead to the dog obsessively licking their skin to the point that it breaks, and acute moist dermatitis, which leads to itchy, weeping skin in patches can also affect the breed. A range of other dermatological conditions may manifest too, including allergies, particularly food allergies, or problems with the thyroid gland which manifest as skin conditions. Cerebellar ataxia Cerebellar ataxia is a hereditary brain condition that is caused by a recessive gene, and usually becomes symptomatic in puppies of between six and twelve weeks old. The condition leads to a range of obvious symptoms and problems, including poor balance and rapid eye movement, as well as problems with focusing. Source: https://www.petmd.com/dog/breeds/c_dg_airedale_terrier \ https://animalhealthcenternh.com/client-resources/breed-info/airedale-terrier Photo credit: https://en.wikipedia.org/wiki/Airedale_Terrier#/media/File:Airedale_Terriers_Flickr.jpg
Breed-related disease: Norwegian Forest Cat

John K. Rosembert The Norwegian Forest cat is a breed of domestic cat originating in Northern Europe. It is a big, strong cat, similar to the Maine Coon breed, with long legs, bushy tail, and sturdy body. The breed is very good at climbing, since they have strong claws they are one of the few domestic cats capable of descending a tree head first With their thick coat of warm, water-resistant fur, the Norwegian Forest Cat is a truly rugged cat. In fact, most experts agree that its ancestors belonged to the Vikings and were used to catch and control vermin on Viking ships. It is also one of the oldest breeds: its ancestors were brought to Norway by Vikings over a thousand years ago and interbred with longhaired cats imported to Norway by Crusaders. True to its name, the Norwegian Forest Cat is built to survive Norway’s cold and snow! Over the centuries, the Norwegian Forest Cat walked Norwegian forests and farms, honing their hunting skills. In 1938, the first Norwegian Forest Cat club was formed to preserve the breed. However, crossbreeding during WWII almost led to the breed’s extinction. Luckily, another official breeding program saved the breed, which didn’t leave Norway until the 1970s. He might have the words “forest cat” in his name, but the Norwegian Forest cat is far from feral. He loves people, in a low-key, cool Norwegian kind of way. He won’t harass you for attention, unless his meals are late but he will follow you around and hang out wherever you are. Their temperament can make him a good choice for families with children and other pets, especially if he has been raised with them. Just make sure children treat him with the gentle respect he deserves. He has an average activity level, not a couch potato but not super-active, either. Below we summarized some of the most common health issues of Norwegian Forest Cat breed in order to help you prevent some predictable risks in your pet. Hypertrophic Cardiomyopathy is the most common heart problem diagnosed in cats. Symptoms include laboured or rapid breathing and lethargy. Although there’s no cure, quality of life can be improved greatly by treatment to control the heart rate and reduce lung congestion. Pyruvate Kinase (PK) is an enzyme deficiency that damages a cat’s red blood cells. The Norwegian Forest is one of the breeds that seems to be more predisposed to it than others. Early signs include anaemia, increased heart rate, muscle wastage and lethargy. Diagnosis involves a full biochemistry profile. Sadly, a bone marrow transplant is the only treatment. Polycystic Kidney Disease can affect Norwegian Forest cats. It’s where lots of fluid-filled cysts develop in the kidneys, leading ultimately to kidney failure. Many cats affected by it won’t display symptoms until middle-age or older and although it’s not curable, supportive treatment can help to minimize the impact for as long as possible. Retinal Dysplasia can affect this breed. Often, this is limited to tiny blind spots over the retina that don’t need to be treated. However, if the dysplasia covers a large area, there’s a greater chance of secondary problems such as cataracts or retinal detachment that will require treatment. Hip Dysplasia is usually an inherited disease that can affect Forest cats. Treatment depends on severity, and in serious cases can involve orthopedic referral and hip surgery. Sources: https://www.everypaw.com/all-things-pet/norwegian-forest-cat-breed-info-health-advice http://www.vetstreet.com/cats/norwegian-forest-cat#personality Photo credit: http://www.vetstreet.com/cats/norwegian-forest-cat#personality https://en.wikipedia.org/wiki/Norwegian_Forest_cat#/media/File:Norwegian_Forest_Cat_in_snow_(closeup)_(cropped).jpg
Direct detection of Ehrlichia canis by PCR in the conjunctiva of a dog with bilateral anterior uveitis-abstract
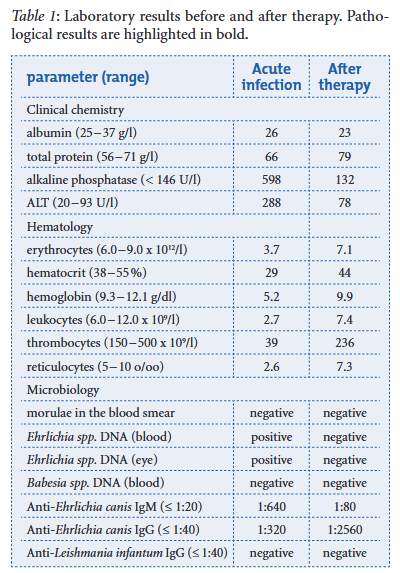
L Walser-Reinhard, D Schaarschmidt-Kiener, J L Forster, F Matheis, B Spiess DOI: 10.1024/0036-7281/a000318 A one-year-old Maltese dog imported from Brazil was presented because of anorexia, dehydration, fever and palpable mandibular lymph nodes. The dog developed clinical signs of bilateral blepharospasm, photophobia and anterior uveitis a few days later. Monocytic ehrlichiosis was diagnosed by positive PCR results from both EDTA blood and conjunctival samples. In addition, Ehrlichia canis-specific IgM and IgG antibodies were both detected. One week after starting treatment with systemic doxycycline and local anti-inflammatory and cycloplegic therapy the dog recovered from systemic and eye diseases. After therapy the follow-up examination revealed a full remission of clinical and hematological parameters and a negative PCR result.
The Thyroid Stimulating Hormone, TSH: Review in Companion Animal

Maigan Espinili Maruquin The serum thyrotropin (thyroid stimulating hormone, TSH) concentration is usually measured in human patients as part of the first-line test for the thyroid function and thus considered best for screening overt and subclinical hyperthyroidism (Ross, Ardisson et al. 1989, Bahn Chair, Burch et al. 2011, Peterson, Guterl et al. 2015). With regards to canine and feline, TSH concentration plays an important role as a biomarker to detect failure of thyroid function, as well. TSH concentration in Canine The hypothyroidism is known to be a common endocrinopathy in dogs. Although it was believed that some cases of canine hypothyroidism were caused by autoimmune thyroiditis, it may also be a result from an inability of the pituitary gland to synthesize and secrete TSH, which results to secondary thyroid follicular atrophy (Ferguson 2007). A classic case of adult-onset hypothyroidism present symptoms of lethargy, weakness, dullness of mental attitude and dermatological problems including alopecia or recurrent skin infections however, in some cases, there are only manifestations of general neuropathy or myopathy (Jaggy and Oliver 1994, Jaggy, Oliver et al. 1994, Ferguson 2007). Being considered as a multisystemic disorder, general medical evaluation should be conducted for suspected cases, including clinicopathologic evaluations (Ferguson DC, Hoenig ME, 1991; Ferguson DC, Hoenig M., 2003) (Ferguson 2007). https://www.horshamvethospital.com.au/hypothyroidism-in-dogs Fig. 01. A canine manifesting signs of hypothyroidism Having false-positive test results are common in hypothyroidism in canines and diagnosis can be challenging, thus, diagnostic testing should be considered to animals presenting clinical and clinicopathologic signs that are consistent with hypothyroidism (McCann 2015). The mostly used diagnostic criteria is with low total or free T4 concentration combined with a high TSH concentration in serum (Dixon and Mooney 1999, Shiel, Sist et al. 2010). The elevated concentration of TSH in dogs with primary hypothyroidism is expected in response to negative feedback of thyroid hormones on the pituitary gland. However, TSH as a sole marker of the disease is not effective due to possibilities of normal TSH in hypothyroid dogs and elevated TSH in euthyroid dogs, resulting to poor sensitivity. Thus, it is usually combined with reduced T4 or free T4 for higher specificity in diagnosis (McCann 2015). TSH concentration in Feline The hyperthyroidism in cats is a common disease in older cats and like in humans, hyperplastic or adenomatous nodular changes in the thyroid are present and peak at the old age (Wakeling, Elliott et al. 2011). This common feline endocrine disease has multiple factors likely involved, including genetic susceptibility (Taylor 2017) and has been diagnosed in 1.5–11.4% of older cats across the world (Carney, Ward et al. 2016, Taylor 2017). Felines with this disorder present signs that vary from the described as classic cat with weight loss, polyphagia, polyuria, polydipsia, increased vocalization, agitation, increased activity, tachypnea, tachycardia, vomiting, diarrhea and an unkempt hair coat, lack of appetite, and lethargy to severely hypermetabolic clinical presentation (Carney, Ward et al. 2016, Taylor 2017). Important comorbidities recorded were cardiorespiratory diseases (Fox, Peterson et al. 1999). A commercial feline-specific thyroid-stimulating hormone (TSH) assay is not yet available in the market, and in some cases, feline samples are analyzed using canine TSH assays, however, delicate differences in TSH at low levels may evade detection. The TSH should always be interpreted with corresponding tT4 or free T4 results (Taylor 2017). An excellent sensitivity is highly suggested if the TSH below the limit of detection is found in a hyperthyroid cat (Peterson ME, 2016)(Taylor 2017). References: Ferguson DC, Hoenig ME. Canine hypothyroidism. In: Allen DG, editor. Small animal medicine. Philadelphia: J.B.Lippincott Co; 1991. p. 845–65. Ferguson DC, Hoenig M. Endocrine system. In: Latimer KS, Mahaffey EA, Prasse KW, editors. Duncan and Prasse’s veterinary laboratory medicine: clinical pathology. 4th edition. Ames (IA): Iowa State Press; 2003. p. 270–303 Peterson ME (2016) Diagnosis and management of iatrogenic hypothyroidism. In: Little SE, ed. August’s Consultations in Feline Medicine Volume 7. Elsevier, St Louis, MO: 260–9 Bahn Chair, R. S., H. B. Burch, D. S. Cooper, J. R. Garber, M. C. Greenlee, I. Klein, P. Laurberg, I. R. McDougall, V. M. Montori, S. A. Rivkees, D. S. Ross, J. A. Sosa and M. N. Stan (2011). “Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists.” Thyroid 21(6): 593-646. Carney, H. C., C. R. Ward, S. J. Bailey, D. Bruyette, S. Dennis, D. Ferguson, A. Hinc and A. R. Rucinsky (2016). “2016 AAFP Guidelines for the Management of Feline Hyperthyroidism.” Journal of Feline Medicine and Surgery 18(5): 400-416. Dixon, R. M. and C. T. Mooney (1999). “Evaluation of serum free thyroxine and thyrotropin concentrations in the diagnosis of canine hypothyroidism.” J Small Anim Pract 40(2): 72-78. Ferguson, D. C. (2007). “Testing for hypothyroidism in dogs.” Vet Clin North Am Small Anim Pract 37(4): 647-669, v. Fox, P. R., M. E. Peterson and J. D. Broussard (1999). “Electrocardiographic and radiographic changes in cats with hyperthyroidism: comparison of populations evaluated during 1992-1993 vs. 1979-1982.” J Am Anim Hosp Assoc 35(1): 27-31. Jaggy, A. and J. E. Oliver (1994). “Neurologic manifestations of thyroid disease.” Vet Clin North Am Small Anim Pract 24(3): 487-494. Jaggy, A., J. E. Oliver, D. C. Ferguson, E. A. Mahaffey and T. G. Jun (1994). “Neurological Manifestations of Hypothyroidism: A Retrospective Study of 29 Dogs.” Journal of Veterinary Internal Medicine 8(5): 328-336. McCann, T. (2015). “Canine hypothyroidism.” Companion Animal 20(10): 572-578. Peterson, M. E., J. N. Guterl, R. Nichols and M. Rishniw (2015). “Evaluation of Serum Thyroid-Stimulating Hormone Concentration as a Diagnostic Test for Hyperthyroidism in Cats.” Journal of Veterinary Internal Medicine 29(5): 1327-1334. Ross, D. S., L. J. Ardisson and M. J. Meskell (1989). “Measurement of thyrotropin in clinical and subclinical hyperthyroidism using a new chemiluminescent assay.” J Clin Endocrinol Metab 69(3): 684-688. Shiel, R. E., M. Sist, R. F. Nachreiner, C. P. Ehrlich and C. T. Mooney (2010). “Assessment of criteria used by veterinary practitioners to diagnose hypothyroidism in sighthounds and investigation of serum thyroid hormone concentrations in healthy Salukis.” Journal of the American Veterinary
Breed-related disease: Border Collie

The classic working farm dog, the Border Collie originated in the border country between Scotland and England. Farmers bred their own individual varieties of sheepdogs for the hilly area. As Borders often tended their flock alone, they had to think independently and be able to run around 50 miles a day in hilly country. Considered highly intelligent, extremely energetic, acrobatic and athletic, they frequently compete with great success in sheepdog trials and dog sports. They are often cited as the most intelligent of all domestic dogs. Border Collies continue to be employed in their traditional work of herding livestock throughout the world and are kept as pets. Border collies are active, working dogs best suited to country living. If confined without activity and company, these dogs can become unhappy and destructive. The breed is highly intelligent, learns quickly and responds well to praise. Border collies are extremely energetic dogs and must have the opportunity to get lots of exercise. They love to run. They also need ample attention from their owners and a job to do, whether that be herding livestock or fetching a ball. They should be socialized well from the time they are young to prevent shyness around strangers, and they should have obedience training, which can help deter nipping behavior and a tendency to run off or chase cars. Below we resume some important diseases more common in your Border Collie. Dental Disease Dental disease is the most common chronic problem in pets affecting 80% of all dogs by age two. Unfortunately, your Border Collie is more likely than other dogs to have problems with her teeth. Dental disease starts with tartar build-up on the teeth and progresses to infection of the gums and roots of the teeth. If we don’t prevent or treat dental disease, your buddy may lose her teeth and be in danger of damaging her kidneys, liver, heart, and joints. In fact, your Border Collie’s life span may even be cut short by one to three years! Cancer Cancer is a leading cause of death in older dogs. Your Collie will likely live longer than many other breeds and therefore is more prone to get cancer in his golden years. Many cancers are curable by surgical removal, and some types are treatable with chemotherapy. Early detection is critical! Multidrug Resistance Multidrug resistance is a genetic defect in a gene called MDR1. If your Border Collie has this mutation, it can affect the way his body processes different drugs, including substances commonly used to treat parasites, diarrhea, and even cancer. For years, veterinarians simply avoided using ivermectin in herding breeds, but now there is a DNA test that can specifically identify dogs who are at risk for side effects from certain medications. Testing your pet early in life can prevent drug-related toxicity. Neurological disorders Although the Border Collie is generally a breed noted for its vitality, they are unfortunately prone to canine epilepsy, a neurological disorder that is the result of an irregular neuroelectric activity. Signs of idiopathic epilepsy include seizures in the form of spasms, twitching, convulsions, and in extreme cases, a loss of consciousness. Idiopathic epilepsy is the most common form of the disease seen in Border Collies. A hereditary condition, IE is usually observed between 6 months and 5 years of age. Heart disorders A congenital heart disease is a common genetic defect that Border Collies are sadly predisposed to, Patent Ductus Arteriosus(POA) is a hereditary abnormality commonly observed in dogs. This heart disease typically leads to an overload of blood on the left side of the heart. In severe cases, it may lead to heart failure and death. Hormonal disorders Another inherited disease that Border Collies are unfortunately subjected to include hypothyroidism, a condition that disrupts the normal production of hormones. You may observe varying signs in a dog affected by this condition, including inactivity or lethargy, weight gain, and hair loss. Once your vet has run a series of tests, if the dog has been diagnosed with this genetic defect, the dog may be placed on medication to regulate their hormonal levels. Sources: http://www.vetstreet.com/dogs/border-collie#health https://www.pet-medcenter.com/storage/app/media/PDF/Dog_pdf/border-collie.pdf Photo Credit: https://en.wikipedia.org/wiki/Border_Collie#/media/File:BORDER_COLLIE,_Simaro_Million_Dollar_Baby_(24290879465)_2.jpg
Leptospirosis and immune-mediated hemolytic anemia: A lethal association
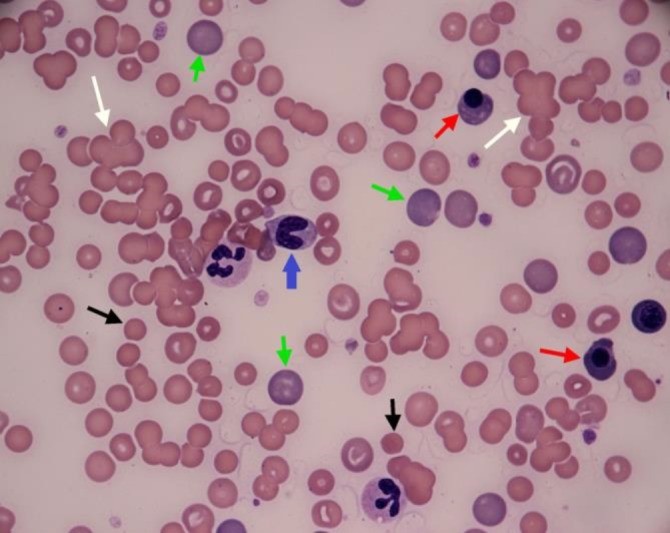
Tommaso Furlanello* and Ida Reale Vet Res Forum. 2019 Summer; 10(3): 261–265. Published online 2019 Sep 15. doi: 10.30466/vrf.2019.99876.2385 An eight-year old crossbreed dog was referred to San Marco Veterinary Clinic with a history of acute illness presenting a severe hemolytic anemia, and intense icterus most likely immune-mediated condition. Circulating antibodies against red blood cells were detected via flow cytometry, while vector-borne diseases were ruled out because of negative results of serological tests for the most common vector-borne diseases in this case. However, leptospirosis was excluded. This resulted in an unsuccessful immunosuppressive therapy with prednisone, two whole blood transfusions and ultimately death of the patient. Leptospirosis was confirmed by both micro-agglutination test for antibodies and PCR test of urine sample. Fig. 1 Blood Smear of the examined dog. White arrows: agglutinates, green arrows: large polycromatophils RBCs, black arrows: spherocytes; red arrow: nucleated RBC, blue arrow: band granulocyte neutrophil. The two-segmented neutrophils visible in the picture display foamy and basophilic cytoplasm, as signs of toxicity, (Diff Quik stain; 100×).
