Dr. Sushant Sadotra
Canine Pancreatitis is one of the most common endocrine diseases occurring in dogs. However, it is more prevalent in dog breeds such as Miniature Schnauzers, Yorkshire Terriers, Cocker Spaniels, Dachshunds, Poodles, and sled dogs.
Pancreatitis, a severe inflammatory condition of the pancreas, can be short-term or long-term, based on the level of pancreatic tissue damage. It can be of acute or chronic type. It can be related to various clinical or subclinical signs and potentially life-threatening.
Causes:
- Dietary indiscretion, such as eating unsuitable food, trash, a high-fat diet, etc., is the most common cause that can be identified in dogs.
- Blunt trauma during a traffic accident or surgery can also cause Pancreatitis.
- High triglycerides (Hypertriglyceridemia) levels in the blood with serum concentrations ≥500 mg/dL can contribute to Pancreatitis.
- Hyperadrenocorticism, hypothyroidism, or other endocrine diseases may also contribute to the onset of Pancreatitis.
- It is also reported that Babesia canis or Leishmania infection can be associated with Pancreatitis in dogs. However, the actual cause and effect are still not very clear.
- Usage of some of the drugs such as cholinesterase inhibitors, calcium, potassium bromide, phenobarbital, l-asparaginase, estrogen, salicylates, azathioprine, thiazide diuretics, vinca alkaloids, etc. may also be linked to Pancreatitis.
Pathogenesis
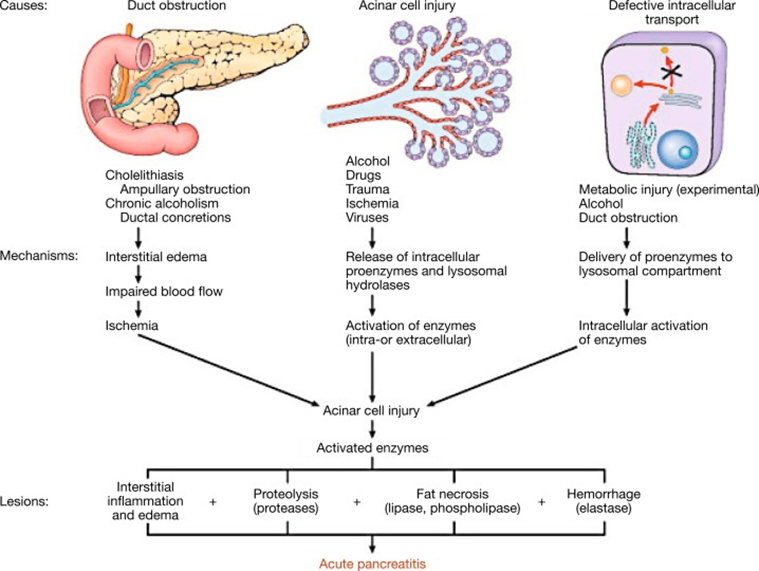
In the initial stages of Pancreatitis, the pancreatic juice is secreted in lesser amounts. Inside the pancreas, a series of steps lead to the activation of pancreatic enzymes. Co-localization of zymogen granules and lysosomes activates trypsinogen to trypsin, which further activates other zymogens. Premature activation of these digestive enzymes causes local damage such as edema, bleeding, inflammation, and necrosis of the pancreas. The inflammation process invites WBCs to the site and increases cytokine production. Altogether, this will cause further damage to pancreases and other distant complications such as generalized inflammation, disseminated intravascular coagulation, disseminated lipodystrophy, hypotension, renal failure, pulmonary failure, myocarditis, etc.
Clinical Findings:
Some of the most common symptoms in dogs are:
- Anorexia (91%)
- Vomiting (90%)
- Weakness (79%),
- Abdominal pain (58%)
- Dehydration (46%)
- Diarrhea (33%)
The milder form of Pancreatitis can be related to subclinical or may have minor or nonspecific signs of anorexia, lethargy, or diarrhea.
Diagnosis:
- Clinical signs of dietary indiscretion, vomiting, and abdominal may indicate the possibility of Pancreatitis in dogs. Suspected cases should be further examined with serum biochemistry profiles, complete blood count, and urinalysis.
- Recently, serum pancreatic lipase immunoreactivity (PLI) concentration has been considered the best clinic pathological test to diagnose canine Pancreatitis.
- Abdominal radiography can allow checking decreased proximal abdominal cavity and displacement of abdominal organs, which can exclude other diseases diagnoses.
- Similarly, abdominal ultrasonography is specific to identifying severe forms of acute Pancreatitis. However, pancreatic enlargement and fluid accumulation around the pancreas may vary the diagnosis. Therefore clinician’s experience plays a critical role.
- Pancreatic cytology, histopathology, or tissue biopsies of the pancreas can be used as definitive diagnostic methods to identify Pancreatitis in dogs.
Among all the methods discussed, histopathology is the gold standard for the diagnosis of canine Pancreatitis. However, a combination of mentioned techniques can be implemented in clinical practice for the most reliable and accurate diagnosis.
Treatment:
Careful monitoring and supportive veterinary care should be given in acute cases to prevent systemic complications.
- In case of vomiting, fluid therapy should be implemented based on the degree of dehydration, ongoing vomiting, or diarrhea. Antiemetic therapy with maropitant (NK1 antagonist), ondansetron, or dolasetron (HT3 antagonists) can help to control vomiting and relieve nausea. If the dog is vomiting frequently and violently, resting the pancreas is suggested by restricting all food or water intake for three to four days.
- Pain medication such as intermittent meperidine, butorphanol, or buprenorphine is usually given to dogs with mild or moderate abdominal pain. Severe pain can be treated with medication such as morphine, fentanyl, or methadone.
- Mild cases of Pancreatitis can also happen due to other risk factors such as hypertriglyceridemia, hypercalcemia, history of medications, or already existing diseases, e.g., cholangitis, hepatitis, inflammatory bowel disease, and diabetes mellitus. Therefore it should also be carefully identified and treated. Feeding a low-fat diet to dogs is essential for successful treatment.
- Other complications related to exocrine pancreatic inefficiency or diabetes mellitus also be closely monitored.
If a dog with chronic pancreatitis has no sign of improvement, additional trial therapy with an immunosuppressive agent such as prednisone, prednisolone, or cyclosporine may be prescribed for the treatment. Treatment for chronic pancreatitis is challenging because of systemic complications such as hypothermia, acidosis, hypocalcemia, and single- or multiple-organ failure.
Reference:
Watson, P. (2015), Pancreatitis in dogs and cats: definitions and pathophysiology. J Small Anim Pract, 56: 3-12.
Whitley EM. Comparative Pancreatic Pathology. Pathobiology of Human Disease. 2014:1101–23. doi: 10.1016/B978-0-12-386456-7.03415-8. Epub 2014 Aug 21. PMCID: PMC7149520.
Xenoulis, P.G. (2015), diagnosis of pancreatitis in dogs and cats. J Small Anim Pract, 56: 13-26.

