Maigan Espinili Maruquin
- Feline NT- proBNP
The atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP) are hormones released into the circulation in response to stimuli. These Natriuretic peptides (NP) are synthesized by cardiomyocytes which regulates body fluid homeostasis and blood pressure (Wilkins, Redondo et al. 1997, Connolly 2010)( Martinez RA, et al., 2009). From preprohormones, NP are processed to prohormones (Blake 2018). The proANP and proBNP, once released, quickly cleaves into separate inactive N-terminal (NT-proANP, NT-proBNP) and active C-terminal (C-ANP, C-BNP) fragments (Oyama 2013, Blake 2018).
In humans, ANP has shorter half- life than the BNP (Suga, Nakao et al. 1992, Blake 2018). On the other hand, while C-terminal provides counterbalance to those of the renin-angiotensin-aldosterone system, it has shorter half-life than that of the N-terminal, making NT-proBNP more stable for assay detection (Potter 2011, Oyama 2013, Blake 2018).
- Hypertrophic Cardiomyopathy (HCM)
The HCM has a prevalence of around 15% among cats wherein this disease of the myocardium causes abnormal thickening of the walls of the left ventricle (LV) (Paige, Abbott et al. 2009, Abbott 2010, Wagner, Fuentes et al. 2010, Payne, Brodbelt et al. 2015, Luis Fuentes and Wilkie 2017). Some cats experiencing HCM develop congestive heart failure (CHF), arterial thromboembolism (ATE), or sudden cardiac death (SCD) (Payne, Borgeat et al. 2013, Payne, Borgeat et al. 2015, Luis Fuentes and Wilkie 2017).
Usually, HCM in felines is detected incidentally on routine veterinary examinations through auscultatory findings including arrhythmias, gallop sounds, or murmurs, while sometimes, detection is from heart failure clinical signs or embolism (Atkins, Gallo et al. 1992, Rush, Freeman et al. 2002, Abbott 2010). Moreover, HCM is considered the most prevalent myocardial disorder in cats (Fox, Liu et al. 1995, Fox, Basso et al. 2007, Paige, Abbott et al. 2009, Fox, Rush et al. 2011).
Due to limited sensitivity and specificity of physical examination, electrocardiography (ECG) and thoracic radiography, diagnosing cardiomyopathy has been a challenge (Côté, Manning et al. 2004, Wood and Picard 2004, Schober, Maerz et al. 2007, Harris, Estrada et al. 2017), whereas, the current clinical gold standard used in cats is echocardiography (Harris, Estrada et al. 2017). Although echocardiography has high specificity in diagnosing myocardial disease (Wood and Picard 2004, Fox, Rush et al. 2011), its sensitivity is sometimes limited in detecting HCM (Fox, Rush et al. 2011).
The efficacy of treatments for the HCM has limited knowledge. Some agents were suspected to slow the progression of HCM in other breeds of cats, considering the probable existence of genetic heterogeneity in feline HCM. Interventions to speed myocardial relaxation or slow heart rate were also observed in attempt to improve diastolic function. (Abbott 2010).
- Feline NT- proBNP Assay
Table 1. Plasma Levels of Feline NT-proBNP and their indications
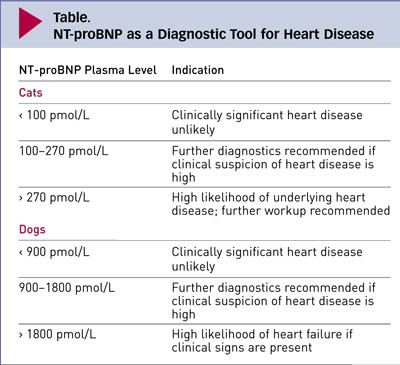
| (https://www.cliniciansbrief.com/article/cardiac-n-terminal-pro-b-type-natriuretic-peptide-assay) |
There is an increase of interest in the usefulness of cardiac biomarker measurement in veterinary practice (Oyama 2013). In cats, there are available, inexpensive, not requiring advance training cardiac biomarkers for initial screening cardiomyopathy (Luis Fuentes and Wilkie 2017)( Charron P., et al., 2003). The echocardiography has a huge role in feline diagnosis of structural heart disease, however, due to its availability and appropriateness in in emergent circumstances, the use of NT-proBNP assays have been stimulated in differentiating CHF and non- cardiac causes of respiratory distress (Oyama, Boswood et al. 2013).
A biomarker is considered clinically useful if it provides information on diagnosis, prognosis, or response to treatment (Oyama 2013). The NT-proBNP in cats can be measured by conducting feline-specific NT-proBNP assay (Singletary, Rush et al. 2012). It has been reported that low NT-proBNP concentration is mostly non- cardiac cause (Oyama 2013) while cats with increased NT-proBNP were reported to have clinically relevant structural heart and elevated concentration suggests CHF (Connolly, Magalhaes et al. 2008, Fox, Oyama et al. 2009, Fox, Rush et al. 2011, Singletary, Rush et al. 2012, Oyama 2013). The NT-proBNP test appears to be not useful for breeding examination (Hsu, Kittleson et al. 2009, Singh, Cocchiaro et al. 2010, Hassdenteufel, Henrich et al. 2013).
References:
Martinez-Rumayor A, Richards AM, Burnett JC, et al. Biology of the natriuretic peptides. Am J Cardiol 2009; 101:3–8.
Charron P, Forissier JF, Amara ME, et al. Accuracy of European diagnostic criteria for familial hypertrophic cardiomyopathy in a genotyped population. Int J Cardiol 2003; 90:33–38
Abbott, J. A. (2010). “Feline Hypertrophic Cardiomyopathy: An Update.” Veterinary Clinics: Small Animal Practice 40(4): 685-700.
Atkins, C. E., A. M. Gallo, I. D. Kurzman and P. Cowen (1992). “Risk factors, clinical signs, and survival in cats with a clinical diagnosis of idiopathic hypertrophic cardiomyopathy: 74 cases (1985-1989).” J Am Vet Med Assoc 201(4): 613-618.
Blake, R. (2018). “The use of cardiac biomarkers in dogs and cats.” Companion Animal 23(10): 569-577.
Connolly, D. J. (2010). “Natriuretic Peptides: The Feline Experience.” Veterinary Clinics: Small Animal Practice 40(4): 559-570.
Connolly, D. J., R. J. Magalhaes, H. M. Syme, A. Boswood, V. L. Fuentes, L. Chu and M. Metcalf (2008). “Circulating natriuretic peptides in cats with heart disease.” J Vet Intern Med 22(1): 96-105.
Côté, E., A. M. Manning, D. Emerson, N. J. Laste, R. L. Malakoff and N. K. Harpster (2004). “Assessment of the prevalence of heart murmurs in overtly healthy cats.” J Am Vet Med Assoc 225(3): 384-388.
Fox, P. R., C. Basso, G. Thiene and B. J. Maron (2007). Spontaneous Animal Models. Arrhythmogenic RV Cardiomyopathy/Dysplasia: Recent Advances. F. I. Markus, A. Nava and G. Thiene. Milano, Springer Milan: 69-78.
Fox, P. R., S. K. Liu and B. J. Maron (1995). “Echocardiographic assessment of spontaneously occurring feline hypertrophic cardiomyopathy. An animal model of human disease.” Circulation 92(9): 2645-2651.
Fox, P. R., M. A. Oyama, C. Reynolds, J. E. Rush, T. C. DeFrancesco, B. W. Keene, C. E. Atkins, K. A. Macdonald, K. E. Schober, J. D. Bonagura, R. L. Stepien, H. B. Kellihan, T. P. Nguyenba, L. B. Lehmkuhl, B. K. Lefbom, N. S. Moise and D. F. Hogan (2009). “Utility of plasma N-terminal pro-brain natriuretic peptide (NT-proBNP) to distinguish between congestive heart failure and non-cardiac causes of acute dyspnea in cats.” J Vet Cardiol 11 Suppl 1: S51-61.
Fox, P. R., J. E. Rush, C. A. Reynolds, T. C. DeFrancesco, B. W. Keene, C. E. Atkins, S. G. Gordon, K. E. Schober, J. D. Bonagura, R. L. Stepien, H. B. Kellihan, K. A. MacDonald, L. B. Lehmkuhl, T. P. Nguyenba, N. Sydney Moise, B. K. Lefbom, D. F. Hogan and M. A. Oyama (2011). “Multicenter Evaluation of Plasma N-Terminal Probrain Natriuretic Peptide (NT-pro BNP) as a Biochemical Screening Test for Asymptomatic (occult) Cardiomyopathy in Cats.” Journal of Veterinary Internal Medicine 25(5): 1010-1016.
Harris, A. N., A. H. Estrada, A. E. Gallagher, B. Winter, K. E. Lamb, M. Bohannon, J. Hanscom and C. A. Mainville (2017). “Biologic variability of N-terminal pro-brain natriuretic peptide in adult healthy cats.” Journal of Feline Medicine and Surgery 19(2): 216-223.
Hassdenteufel, E., E. Henrich, N. Hildebrandt, A. Stosic and M. Schneider (2013). “Assessment of circulating N-terminal pro B-type natriuretic peptide concentration to differentiate between cardiac from noncardiac causes of pleural effusion in cats.” Journal of Veterinary Emergency and Critical Care 23(4): 416-422.
Hsu, A., M. D. Kittleson and A. Paling (2009). “Investigation into the use of plasma NT-proBNP concentration to screen for feline hypertrophic cardiomyopathy.” J Vet Cardiol 11 Suppl 1: S63-70.
Luis Fuentes, V. and L. J. Wilkie (2017). “Asymptomatic Hypertrophic Cardiomyopathy: Diagnosis and Therapy.” Veterinary Clinics: Small Animal Practice 47(5): 1041-1054.
Oyama, M. A. (2013). “Using Cardiac Biomarkers in Veterinary Practice.” Veterinary Clinics: Small Animal Practice 43(6): 1261-1272.
Oyama, M. A., A. Boswood, D. J. Connolly, S. J. Ettinger, P. R. Fox, S. G. Gordon, J. E. Rush, D. D. Sisson, R. L. Stepien, G. Wess and F. Zannad (2013). “Clinical usefulness of an assay for measurement of circulating N-terminal pro-B-type natriuretic peptide concentration in dogs and cats with heart disease.” Journal of the American Veterinary Medical Association 243(1): 71-82.
Paige, C. F., J. A. Abbott, F. Elvinger and R. L. Pyle (2009). “Prevalence of cardiomyopathy in apparently healthy cats.” Journal of the American Veterinary Medical Association 234(11): 1398-1403.
Payne, J. R., K. Borgeat, D. C. Brodbelt, D. J. Connolly and V. Luis Fuentes (2015). “Risk factors associated with sudden death vs. congestive heart failure or arterial thromboembolism in cats with hypertrophic cardiomyopathy.” Journal of Veterinary Cardiology 17: S318-S328.
Payne, J. R., K. Borgeat, D. J. Connolly, A. Boswood, S. Dennis, T. Wagner, P. Menaut, I. Maerz, D. Evans, V. E. Simons, D. C. Brodbelt and V. Luis Fuentes (2013). “Prognostic Indicators in Cats with Hypertrophic Cardiomyopathy.” Journal of Veterinary Internal Medicine 27(6): 1427-1436.
Payne, J. R., D. C. Brodbelt and V. Luis Fuentes (2015). “Cardiomyopathy prevalence in 780 apparently healthy cats in rehoming centres (the CatScan study).” Journal of Veterinary Cardiology 17: S244-S257.
Potter, L. R. (2011). “Natriuretic peptide metabolism, clearance and degradation.” Febs j 278(11): 1808-1817.
Rush, J. E., L. M. Freeman, N. K. Fenollosa and D. J. Brown (2002). “Population and survival characteristics of cats with hypertrophic cardiomyopathy: 260 cases (1990-1999).” J Am Vet Med Assoc 220(2): 202-207.
Schober, K. E., I. Maerz, E. Ludewig and J. A. Stern (2007). “Diagnostic accuracy of electrocardiography and thoracic radiography in the assessment of left atrial size in cats: comparison with transthoracic 2-dimensional echocardiography.” J Vet Intern Med 21(4): 709-718.
Singh, M. K., M. F. Cocchiaro and M. D. Kittleson (2010). “NT-proBNP measurement fails to reliably identify subclinical hypertrophic cardiomyopathy in Maine Coon cats.” J Feline Med Surg 12(12): 942-947.
Singletary, G. E., J. E. Rush, P. R. Fox, R. L. Stepien and M. A. Oyama (2012). “Effect of NT-pro-BNP Assay on Accuracy and Confidence of General Practitioners in Diagnosing Heart Failure or Respiratory Disease in Cats with Respiratory Signs.” Journal of Veterinary Internal Medicine 26(3): 542-546.
Suga, S., K. Nakao, K. Hosoda, M. Mukoyama, Y. Ogawa, G. Shirakami, H. Arai, Y. Saito, Y. Kambayashi, K. Inouye and et al. (1992). “Receptor selectivity of natriuretic peptide family, atrial natriuretic peptide, brain natriuretic peptide, and C-type natriuretic peptide.” Endocrinology 130(1): 229-239.
Wagner, T., V. L. Fuentes, J. R. Payne, N. McDermott and D. Brodbelt (2010). “Comparison of auscultatory and echocardiographic findings in healthy adult cats.” Journal of Veterinary Cardiology 12(3): 171-182.
Wilkins, M. R., J. Redondo and L. A. Brown (1997). “The natriuretic-peptide family.” Lancet 349(9061): 1307-1310.
Wood, M. J. and M. H. Picard (2004). “Utility of echocardiography in the evaluation of individuals with cardiomyopathy.” Heart (British Cardiac Society) 90(6): 707-712.

