KNOWING THE THREAT OF CANINE BABESIOSIS
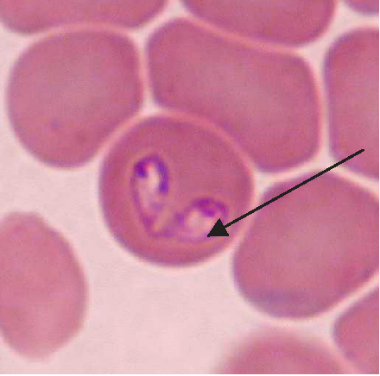
Maigan Espinili Maruquin Our pets are members of our family. And like the other members, they need care, love, and attention. We spend most of our time in the work, school, and other daily activities we have, which lessens the time we spend with our pets. However, we should also listen to our companions who stays at home. Attend to their needs, specially their health. As important as the humans, dogs also need regular medical checks to make sure that they are living a happy and healthy life. One of the diseases you should be cautious of when you have a dog companion are those caused by parasites. For both domestic and wild canines, canine babesiosis is an important widespread disease. The disease is caused by single-celled microorganisms (protozoa) belonging to the Babesia family. Babesia parasites are primarily spread by the bite of an infected tick. The distribution of the canine Babesia species are greatly affected by the presence of tick vector species in the area. Babesia infecting dogs are morphologically classified into forms of large, including B. canis, B. volgeli, B. rossi, and small, including B. gibsoni, both exhibiting a worldwide distribution. Among Babeisa species infecting dogs, B. gibsoni has been recognized as an important pathogen that affects dogs in the Middle East, Africa, Asia, Europe, and many areas of the United States. The babesiosis is associated mainly in haemolytic anaemia or the destruction and breaking down of the red blood cells. B. gibsoni can cause hyperacute, acute, and chronic infections. Clinical signs present are ambiguous, which includes depression, lethargy, fever, weakness, vomiting, pale gums and anorexia. However, other specific signs include dark coloration of the urine, neurological dysfunction, respiratory failure, jaundice, and sometimes presence of bleeding diatheses. Severe cases may lead to organ failure and death. However, some cases during the initial stages appear to be unnoticed to the pet owners. On the other hand, chronic stages often make the dog a carrier of the organism and becomes asymptomatic, and for how long will a dog be a carrier is unknown. How do dogs get infected with babesiosis? The Babesia species resides in its first host, the tick vector. Dogs become infected when ticks feed for 2 to 3 days and release sporozoites, from the salivary gland, into the circulation of dogs. Inside the host, sporozoites start to invade red blood cells, and replicate via binary fission, which produces merozoites to further invade other red blood cells. Ticks become infected with merozoites during feeding, and sexual reproduction of Babesia’s life cycle completes within the ticks. In addition, transmission can also occur through transfusion of infected blood, transplacental transmission (to unborn puppies in the uterus of their mothers), or direct blood-blood contact during fighting. How is babesiosis diagnosed? Canine babesiosis is historically identified based on the observation of the parasite within red blood cells using light microscope. Infection of large or small form of Babesia can be morphagically identified, if enough parasites present in the blood, in the blood smear. Other diagnostic tests detecting antigen include FA (fluorescent antibody) staining of the organism and PCR (polymerase chain reaction) detecting nucleic acid of the Babesia. The PCR test has the advantage in that it can identify all four species of Babesia, but requires trained persons to run it. Serologic or antibody testing may also be performed to see the presence of the parasite. Antibody reaction to the Babesia infection can be measured by ELISA (enzyme-linked immunosorbent assay) in the lab. In addition, a lateral flow immunochromatographic test (or rapid test) has been developed to provide a fast and in-site assay to detect the antibody of dogs infected with B. gibsoni. This rapid test has been commonly assisting the veterinarians for fast diagnosis. Disease Management and Prevention The treatment of an infected dog consists of three components: antiprotozoal treatment of babesiosis, blood transfusions to treat severe anaemia, and supportive therapies for the complications and metabolic derangements. Meanwhile, as a pet owner, regular control of the tick vectors by routinely dipping or spraying pets or using tick collars or spot-on preparations is the only effective way of preventing this disease in most parts of the world. Ticks,if founed on your pets, shouldn’t be squeezed, crushed or twisted to avoid the parasite from being expelled. Removing it properly shall be done or ask the assistance of your veterinarians. To take the ticks off your dog, tick’s mouth should be grasped as close to the skin as possible using forceps. Tick’s mouth shall be removed as much as possible. Afterwhich, make sure to clean the tick bitten area with soap and water or using mild antibacterial wound cleanser. In addition, preventing dogfighting as well as direct blood contact by using sterilized instruments during tail docking and ear cropping procedures and when administering injections are critical. Moreover, a vaccine against B. canis has become commercially available in some countries. You may check with your pet’s veterinarians prior to visiting endemic areas with your dogs. Fig. 1. Two pear-shaped Babesia canis organisms in an erythrocyte. (Duh et al., 2004) Fig. 2. Babesia gibsoni in erythrocytes in a blood smear stained with modified Wright technique. (Trotta et al., 2009) Chauvin A., Moreau E., Bonnet S., Plantard O. & Malandrin L. Babesia and its hosts: adaptation to long-lasting interactions as a way to achieve efficient transmission. 2009. Vet. Res., 40 (2), 37.64. Duh D, Tozon N, Petrovec M, Strasek K, Avsic-Zupanc T. Canine babesiosis in Slovenia: molecular evidence of Babesia canis canis and Babesia canis vogeli. 2004. Vet Res. 35(3):363-8. Refer Conrad P., Thomford J., Yamane I., Whiting J., Bosma L., Uno T., Holshuh H.J. & Shelly S. Hemolytic anemia caused by Babesiagibsoni infection in dogs. 1991. J. Am. Vet. Med. Assoc., 199 (5): 601–605. Trotta M, Carli E, Novari G, Furlanello T, Solano-Gallego L. Clinicopathological findings, molecular detection and characterization of Babesia gibsoni infection in a sick dog from Italy. 2009. Vet Parasitol. 165(3-4):318-22.
Case report: systemic tuberculosis caused by Mycobacterium bovis in a cat- Abstract
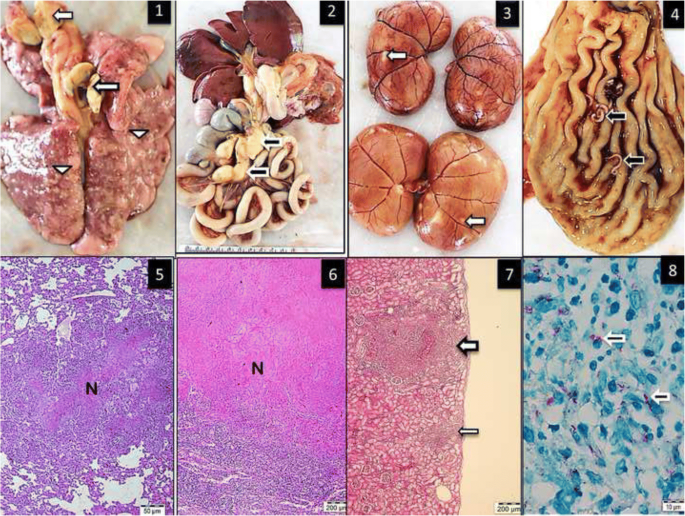
Source: https://bmcvetres.biomedcentral.com/articles/10.1186/s12917-018-1759-7 Mycobacterium bovis was isolated from the lungs, bronchial and gastrointestinal lymph nodes, kidney and liver of a 5-year-old stray male cat. The isolate was confirmed as M. bovis using the Genotype MTBC assay (Hain Lifescience, Germany), which allows differentiation of species within the Mycobacterium tuberculosis complex. The Systemic tuberculosis was diagnosed via postmortem examination of the cat. Pathological changes included multifocal to coalescing granulomatous inflammation in the lungs, liver, lymph nodes and kidneys. Infection by immunosuppressive viral pathogens including feline herpes virus-1, feline immunodeficiency virus and feline parvovirus virus were ruled out by polymerase chain reaction assay (PCR). The isolated M. bovis was susceptible to isoniazid, ethambutol, rifampicin or streptomycin. Unlike previous cases of feline tuberculosis in Turkey, this case report details the first case of feline tuberculosis in Turkey for which the causative agent (M. bovis) was confirmed with bacteria isolation, morphological evaluation, molecular characterization and antibiotic sensitivity. Figure Multifocal granulomatous pneumonia (arrowhead) and diffuse lymphadenitis (arrow) of tracheobronchial lymph nodes. 2. Diffuse, severe lymphadenitis in mesenteric lymph nodes (arrow). 3. Multifocal granulomatous nephritis. 4. Gastric worms on the mucosal surface (arrows). 5.6.7. Granulomatous pneumonia (5) with necrosis (N), lymphadenitis (6) and necrosis and nephritis (7) with granulomas (arrows), HE. 8. Acid-fast microorganisms in the cytoplasm of epithelioid macrophages (arrows), ZN
Breed-related disease: Saint Bernard

The St. Bernard or St Bernard is a breed of very large working dog originated in Switzerland along with several other breeds, including the Bernese Mountain Dog, Entlebuch Cattle Dog, Appenzell Cattle Dog, and Greater Swiss Mountain Dog. They probably were created when dogs native to the Alps were crossed with Mastiff-type dogs that came with the Roman army during the time of the emperor Augustus. By the first millennium CE, dogs in Switzerland and the Alps were grouped together and known simply as Talhund” (Valley Dog) or “Bauernhund” (Farm Dog). The Saint Bernard is one of the most popular giant breeds. Its powerful and muscular build contrasts the wise, calm expression. The breed has either long or short hair, ranging in color from a deep to a more yellowed brown, with white markings always present. Even though the Saint Bernard is not very playful, it is patient, gentle, and easy-going with children. It is willing to please and shows true devotion to its family. Sometimes the dog displays its stubborn streak. The Saint Bernard breed, which has a lifespan of 8 to 10 years, may suffer from major health problems such as: Hip Dysplasia: This is a heritable condition in which the thighbone doesn’t fit snugly into the hip joint. Some dogs show pain and lameness on one or both rear legs, but you may not notice any signs of discomfort in a dog with hip dysplasia. Entropion: This defect, which is usually obvious by six months of age, causes the eyelid to roll inward, irritating or injuring the eyeball. One or both eyes can be affected. If your Saint has entropion, you may notice him rubbing at his eyes. The condition can be corrected surgically. Epilepsy: This disorder causes mild or severe seizures. Epilepsy can be hereditary; it can be triggered by such events as metabolic disorders, infectious diseases that affect the brain, tumors, exposure to poisons, or severe head injuries; or it can be of unknown cause (referred to as idiopathic epilepsy). Osteochondrosis; is another inherited orthopedic condition that can affect Saints and many other breeds. It’s a defect in the formation of growing cartilage that causes it to fragment. It usually appears in dogs younger than 1 year. Sources: https://dogtime.com/dog-breeds/saint-bernard#/slide/1 Photo credit : http://www.vetstreet.com/dogs/saint-bernard#health
Breed-related disease: Savannah Cat

The Savannah cat is the largest of the cat breeds. A Savannah cat is a cross between a domestic cat and a serval, a medium-sized, large-eared wild African cat. The unusual cross became popular among breeders at the end of the 1990s, and in 2001 The International Cat Association (TICA) accepted it as a new registered breed. In May 2012, TICA accepted it as a championship breed. Some states restrict the ownership of the Savannah to the later filial ratings. A great deal of a Savannah’s personality may depend on how close they are to their F1 cross. A Savannah can be black, brown spotted tabby, black silver spotted tabby or black smoke. Black Savannahs are solid black but may have faint “ghost spots” that can be seen beneath the black color. Some are very social and friendly with new people, while others may run and hide or revert to hissing and growling when seeing a stranger. Savannahs have strong hunting instincts and love to climb and jump. Early socialization is crucial to their development. Well socialized Savannah’s can be affectionate and playful members of the family. This guide contains general health information important to all felines as well as information on genetic predispositions for Savannahs. Here we gathered some of the most common diseases in Savannah Heart Disease Cardiomyopathy is the medical term for heart muscle disease, either a primary inherited condition or secondary to other diseases that damage the heart. The most common form called hypertrophic cardiomyopathy, or HCM, is a thickening of the heart muscle often caused by an overactive thyroid gland. Arterial Thromboembolism Cats with heart disease may develop blood clots in their arteries known as FATE (feline aortic thromboembolisms). Blood clots most commonly become lodged just past the aorta, the large blood vessel that supplies blood from the heart to the body, blocking normal blood flow to the hind legs. When this happens, one or both hind legs may become paralyzed, cold, or painful. FLUTD When your cat urinates outside the litter box, you may be annoyed or furious, especially if your best pair of shoes was the location chosen for the act. But don’t get mad too quickly—in the majority of cases, cats who urinate around the house are sending signals for help. Although true urinary incontinence, the inability to control the bladder muscles, is rare in cats and is usually due to improper nerve function from a spinal defect, most of the time, a cat that is urinating in “naughty” locations is having a problem and is trying to get you to notice. What was once considered to be one urinary syndrome has turned out to be several over years of research, but current terminology gathers these different diseases together under the label of Feline Lower Urinary Tract Diseases, or FLUTD. Allergies/Atopy In humans, an allergy to pollen, mold, or dust makes people sneeze and their eyes itch. In cats it makes the skin itchy. We call this form of allergy “atopy.” Commonly, the legs, belly, face, and ears are very likely to have this problem. Symptoms typically start between the ages of one and three and can get worse every year. Source: https://aubreyamc.com/feline/savannah/ Photo Credit : https://animalhealthcenternh.com/client-resources/breed-info/savannah/ http://www.vetstreet.com/cats/savannah
