Case study: Coinfection with Tritrichomonas foetus and Giardia duodenalis in Two Cats with Chronic Diarrhea
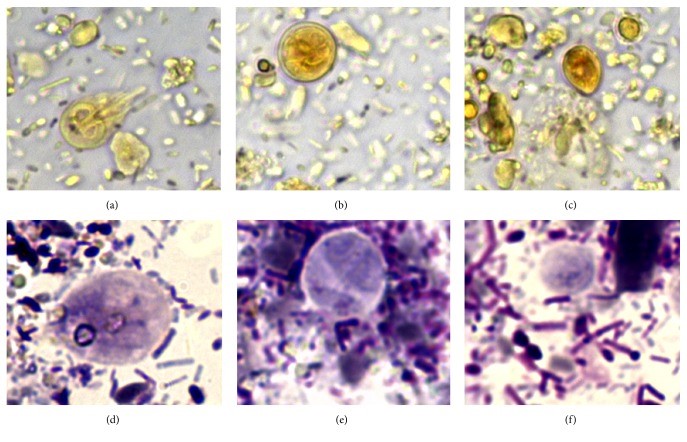
Case study: Coinfection with Tritrichomonas foetus and Giardia duodenalis in Two Cats with Chronic Diarrhea Robert Lo, Ph.D, D.V.M A mixed infection of Tritrichomonas foetus and Giardia duodenalis was confirmed in two 6-year-old Maine Coon cats. One of the cats had a history of chronic liquid diarrhea and several treatment failures. Both cats observed G. duodenalis and trichomonas from the fecal smears, and the infection of T. foetus was also confirmed by RT-PCR. The cat recovered completely after taking ronidazole treatment. In refrigerated stool specimens collected from cats with chronic diarrhea, drop-shaped trichomonad pseudocysts, which are smaller than the cysts of G. duodenalis, were detected. When the pseudocysts are stained with Lugol’s solution or Giemsa, they appear brown or light blue, respectively, and their morphological characteristics are similar to those of bovine T. foetus in vitro. It is worth noting that the pseudocysts in feline trichomonads may be a way for the protozoa to fight against unfavorable environments. Clinicians detected pseudocysts in refrigerated stool, which may be a useful clues to the diagnosis of this disease. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6005279/ Figure 1 Fecal smears of a 6-month-old female Maine Coon cat with chronic liquid diarrhea, stained with Lugol’s solution (a–c) and Giemsa stain (d–f); showed (a) and (d) Giardia duodenalis trophozoites ; (B) and (e) a Giardia duodenalis cyst; (c) and (f) drop-shaped trichomonads (630x). Fecal smears from a 6-month-old female Maine Coon cat with chronic liquid diarrhea stained with Lugol’s solution (a–c) and Giemsa stain (d–f); (a) and (d) showed Giardia duodenalis trophozoite; (b) and (e) showed a Giardia duodenalis cyst; (c) and (f) showed drop-shaped trichomonads (630x). Figure 2 Trichomonads in fecal smear from the cat with diarrhea. Arrow heads in (a) indicate anterior flagella emerging from the trophozoite, while arrow heads in (b) indicate undulating membrane (1000x). Figure 3 Typical morphology of trichomonads observed in saline solution-diluted fresh fecal smear from the cat with diarrhea. Arrow heads in (a) and in (b) indicate anterior flagella and undulating membrane, respectively (630x). Figure 4 Drop-shaped unidentified elements in fecal smears stained with Lugol’s solution (a) and Giemsa stain (b-c). Arrow heads in (a) indicate an internal oval structure (400x). Arrow heads in (b) indicate a curved linear structure (1000x). Arrow heads in (c) indicate an undulated portion of the surface (1000x).
Toxoplasmosis In Cats: A Review
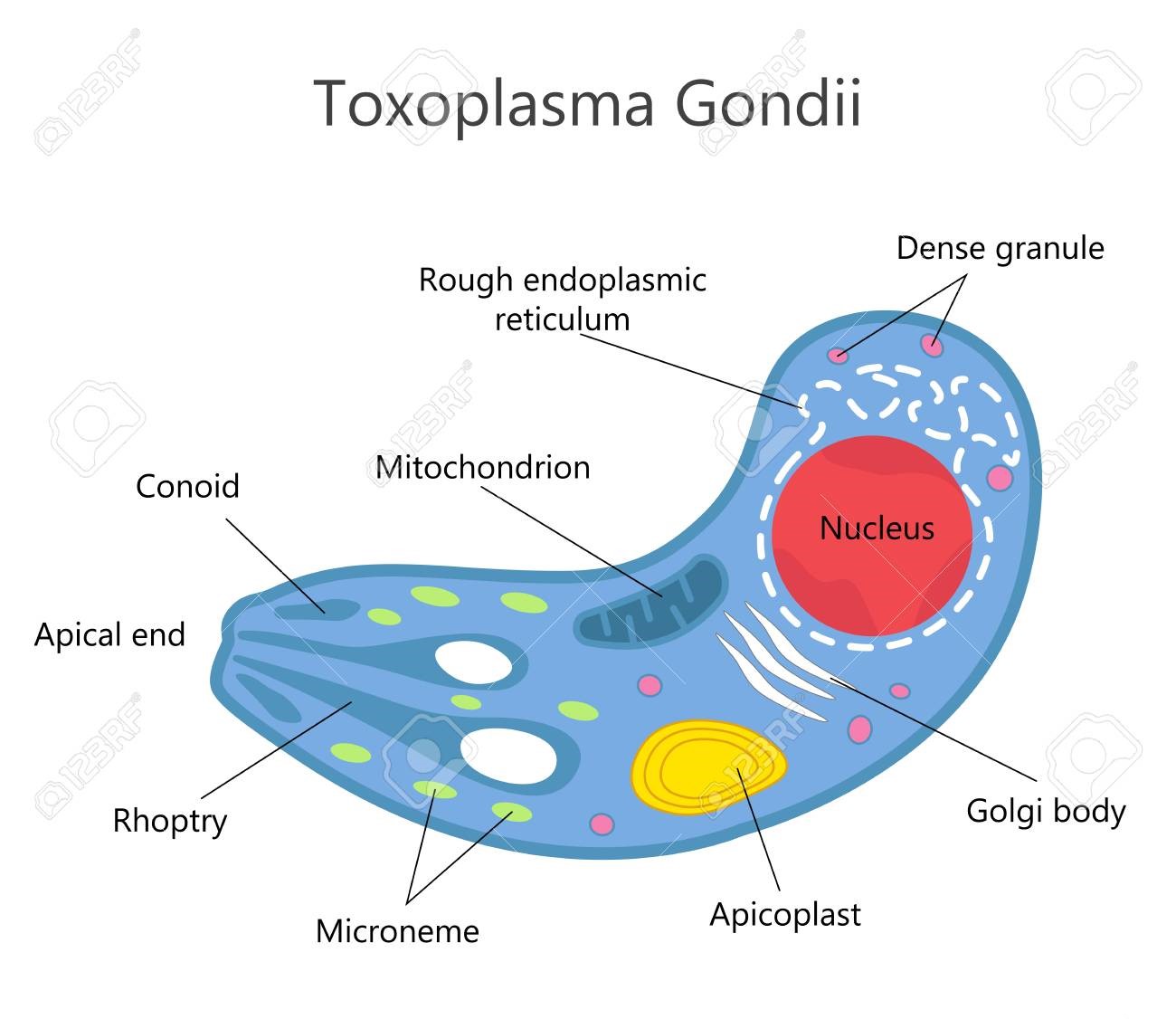
Toxoplasmosis In Cats: A Review. Maigan Espinili Maruquin Structure and Replication Fig. 01 Structure of Toxoplasma gondii (https://www.123rf.com/photo_81668845_stock-vector-toxoplasma-gondii-structure-.html) The family Felidae is the only animal species that hosts infective oocysts of Toxoplasma gondii and passes through their feces, however, this parasite infects most species of birds and mammals (Elmore, Jones et al. 2010). This pathogen is an obligate intracellular coccidian parasite an can infect warm-blooded animals, including people (Hartmann, Addie et al. 2013) (Dubey JP, 2005; Dubey JP and Lappin MR, 2006). The complex life cycle of T. gondii undergoes three distinguished stages. The tachyzoites, formerly called the trophozoite or endozoite, is the active multiplying stage and most likely to cause clinical disease and spread to almost all organs. The next stage is the bradyzoite stage where multiplication is slow and usually within a tissue cyst, leading to a life-long chronic infection. This stage penetrates the small intestine epithelial cells. Finally, the oocysts, which are excreted and shed in feces of infected felid, are the result of sexual reproduction within the intestine and constitute the environmentally resistant stage. (Dubey JP, 2005; Dubey JP and Lappin MR, 2006) (Dabritz, Gardner et al. 2007, Dabritz, Miller et al. 2007, Hartmann, Addie et al. 2013, Wyrosdick and Schaefer 2015, Calero-Bernal and Gennari 2019). Oocysts are non- infectious when excreted in feces but begin to become sporulate after 1-5 days of exposure to air and moisture. These are round to oval in shape and around 10 x 12 μm in size. Most naïve cats who get infected take 3–10 days of ingestion of tissue cysts to complete the cycle (Hartmann, Addie et al. 2013) (Dubey JP, 2005; Dubey JP and Lappin MR, 2006). Infection/ Pathogenesis The very first case of toxoplasmosis in cats was diagnosed from a domestic cat in Middletown, NY, in 1942 (Olafson and Monlux, 1942; Dubey, 2008)(Wyrosdick and Schaefer 2015). Generally, most cats at 6 to 10 weeks were detected to have antibodies to T. gondii while maternally transferred antibodies (MTAs) disappear by 12 weeks of age. Seropositivity increases with the age and varies according to the cat’s lifestyle (like hunting food) (Dubey, J.P., 2010)(Dubey, Cerqueira-Cézar et al. 2020). The oocysts were noted to remain infectious in the environment for at least 12 months (Hutchison 1965, Wyrosdick and Schaefer 2015). Generally, transmissions of the parasite are congenital infection, ingestion of the infected tissue, and ingestion of oocyst-contaminated food or water (Dubey JP and Lappin MR., 2006) (Hartmann, Addie et al. 2013). Most likely, congenitally infected kittens show clinical signs while post-natal infections are usually through ingestion of infected tissue cysts and in some cases, oocysts (Dubey and Jones 2008, Elmore, Jones et al. 2010). Queens giving birthe to infected kittens during gestation can become infected transplacentally or via suckling (Dubey JP, et al., 1996) (Calero-Bernal and Gennari 2019) The most common method of feline infection due to predation of intermediate hosts is tissue cyst ingestion where shedding occurs in 3 to 5 days, while ingestion of tachyzoites takes 8- 10 days, and 21-24 days after ingestion of oocysts (Dubey, J.P., 2010) (Schares, Vrhovec et al. 2008, Wyrosdick and Schaefer 2015). Clinical Signs Feline toxoplasmosis develops clinical signs rarely but causes inflammation and tissue necrosis from intracellular growth of tachyzoites (Dubey JP and Lappin MR, 2006)(Hartmann, Addie et al. 2013). It frequently results to hepatitis, pneumonia, and encephalitis with signs of ascites, lethargy, and dyspnea while infected adults do not show specific clinical signs (Brennan A, et al, 2016) (Dubey and Carpenter 1993, Calero-Bernal and Gennari 2019). Moreover, observations also showed extra- intestinal enteritis (Cohen, Blois et al. 2016) and inflammatory intestinal disease (Peterson, Willard et al. 1991). Tissues that are most commonly affected are the central nervous system, the muscles, the lungs, and the eyes. Infected cats show neurological signs, muscle hyperesthesia, jaundice, diarrhea, fever, depression, anorexia, vomiting, paresis, dermatitis and weight loss (Dubey JP and Lappin MR, 2006) (Hartmann, Addie et al. 2013, Dubey, Cerqueira-Cézar et al. 2020). When severe respiratory and neurological signs were observed, it’s usually fatal (Dubey and Carpenter 1993). Diagnosis Diagnosis in cats for toxoplasmosis include ante-mortem fecal examination for oocysts and serologic testing (Johnson, Tinker et al. 2009, Elmore, Jones et al. 2010). However, geographical location may influence differential diagnosis (Calero-Bernal and Gennari 2019). The shedding of the oocysts of an infected cats may only be once in their lifetime (Elmore, Jones et al. 2010) which can be diagnosed in their fecal samples via microscopy (Hartmann, Addie et al. 2013). However, there is low probability of finding oocysts in the fecal samples of infected cats and there is a confusing morphological resemblance of the T. godii oocysts to other coccidian like Hammondia hammondi and Besnoitia spp (Elmore, Jones et al. 2010). Therefore, molecular and bioassay techniques can be used to distinguish them while only mouse bioassay is the definitive confirmation method (Dubey 2009, Elmore, Jones et al. 2010). In diagnosing T. gondii, confirmation is when the organism is found in body fluids or tissue (Hartmann, Addie et al. 2013). For tachyzoites detection, ante- mortem diagnosis in tissues and body fluids during acute illness may use cytology or polymerase chain reaction (PCR). A definitive diagnosis is when tachyzoites were detected rarely in blood but aqueous humour, lymph nodes, and transtracheal or bronchoalveolar lavage fluid can be used (Hartmann, Addie et al. 2013). On the other hand, antibodies of the IgM, IgG and IgA isotypes can be detected by immunofluorescence assay (IFA). For antibody- negative, cats are likely to shed oocysts while antibody- positive cats don’t shed oocysts wherein antibodies need 2–3 weeks to develop (Dubey JP, 2005)(Hartmann, Addie et al. 2013). Despite the development of immunofluorescence and ELISA tests, requirement for species-specific protein conjugate makes it limitedly used in veterinary diagnostics (Wyrosdick and Schaefer 2015). After comparing indirect hemagglutination test, latex agglutination test, Feldman dye test and modified agglutination tests, the aqueous humour resulted to be the most sensitive of
Heartworm in Cats
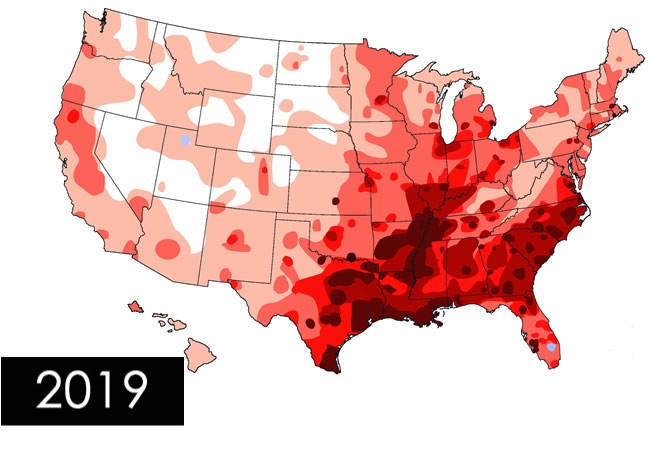
Heartworm in Cats Andy Pachikerl, Ph.D Introduction of Feline Heartworm Heartworm disease is a serious and potentially fatal disease in pets worldwide and it is caused by foot-long worms (heartworms) that dwells in the heart, lungs, and associated blood vessels of affected pets. This in turn cause severe lung disease, heart failure and damage to other organs in the body. Heartworm disease affects dogs, cats, and ferrets, but heartworms also live in other mammal species, including wolves, coyotes, foxes, sea lions and—in rare instances—humans. Because wild species such as foxes and coyotes live in proximity to many urban areas, they are considered important carriers of the disease (Ettinger, et al., 2010). Among mammalian definitive hosts, they are best adapted to domesticated and wild dogs. If untreated, their numbers can increase, and dogs have been known to harbour several hundred worms in their bodies. Heartworm disease causes lasting damage to the heart, lungs, and arteries, and can affect the dog’s health and quality of life long after the parasites are gone (2019). For this reason, prevention is by far the best option, and treatment—when needed—should be administered as early in the course of the disease as possible. Heartworm disease in cats is quite distinctive from heartworm disease in dogs. Since cat is an atypical host for heartworms, most worms in cats do not survive to the adult stage. Cats with adult heartworms usually have just one to three worms, and many cats affected by heartworms have no adult worms. Even if feline host of heartworm rarely occurs, cat heartworm disease often goes undiagnosed. Therefore, it is important to understand that even immature worms cause real damage in the form of a condition known as heartworm associated respiratory disease (HARD). Moreover, the medication used to treat heartworm infections in dogs cannot be used in cats, so prevention is the only means of protecting cats from the effects of heartworm disease (Society, 2007). Transmission Figure 1. Diagram from American Heartworm Society showing how the heartworm is spread and inter-transmission can occur via different host pets. The mosquito plays an essential role in the heartworm life cycle. Adult female heartworms living in an infected dog, fox, coyote, or wolf produce microscopic baby worms called microfilaria that circulate in the bloodstream. When a mosquito bites and takes a blood meal from an infected animal, it picks up these baby worms, which develop and mature into “infective stage” larvae over a period of 10 to 14 days (Johnstone, 1998). Then, when the infected mosquito bites another dog, cat, or susceptible wild animal, the infective larvae are deposited onto the surface of the animal’s skin and enter the new host through the mosquito’s bite wound. Once inside a new host, it takes approximately 6 months for the larvae to mature into adult heartworms. Once mature, heartworms can live for 5 to 7 years in dogs and up to 2 or 3 years in cats. Because of the longevity of these worms, each mosquito season can lead to an increasing number of worms in an infected pet (Knight, et al., 1998). Symptoms and signs of heartworm in cats Signs of heartworm disease in cats can be of two extremes: very subtle or plain out dramatic. Symptoms may include coughing, asthma-like attacks, periodic vomiting, lack of appetite, or weight loss. Occasionally an affected cat may have difficulty walking, experience fainting or seizures, or suffer from fluid accumulation in the abdomen. Unfortunately, the first sign in some cases is collapse of the cat, or sudden death (Society, 2007). How significant is my cat’s risk for heartworm infection? Figure 2. Diagram showing the severity of heartworms in the USA as shown by the American Heartworm Society Many factors must be considered, even if heartworms do not seem to be a problem in your local area. Your community may have a greater incidence of heartworm disease than you realize—or you may unknowingly travel with your pet to an area where heartworms are more common. Heartworm disease is also spreading to new regions of the country each year. Stray and neglected dogs and certain wildlife such as coyotes, wolves, and foxes can be carriers of heartworms. Mosquitoes blown great distances by the wind and the relocation of infected pets to previously uninfected areas also contribute to the spread of heartworm disease (this happened following Hurricane Katrina when 250,000 pets, many of them infected with heartworms, were “adopted” and shipped throughout the country). The fact is that heartworm disease has been diagnosed in all 50 states, and risk factors are impossible to predict. Multiple variables, from climate variations to the presence of wildlife carriers, cause rates of infections to vary dramatically from year to year—even within communities. And because infected mosquitoes can come inside, both outdoor and indoor pets are at risk. For that reason, the American Heartworm Society recommends that you “think 12:” (1) get your pet tested every 12 months for heartworm and (2) give your pet heartworm preventive 12 months a year. Diagnosis Heartworm disease is a serious, progressive disease. The earlier it is detected, the better the chances the pet will recover. There are few, if any, early signs of disease when a dog or cat is infected with heartworms, so detecting their presence with a heartworm test administered by a veterinarian is important. The test requires just a small blood sample from your pet, and it works by detecting the presence of heartworm proteins. Some veterinarians process heartworm tests right in their hospitals while others send the samples to a diagnostic laboratory. In either case, results are obtained quickly. If your pet tests positive, further tests may be ordered (Yin, 2007). Diagnosis period Heartworm infection in cats is harder to detect than in dogs, because cats are much less likely than dogs to have adult heartworms. The preferred method for screening cats includes the use of both an antigen and an antibody test (the “antibody”
Breed-related disease: The Rottweiler

John K. Rosembert The Rottweiler is a breed of domestic dog regarded as medium-to-large, or large. The dogs were known in German as Rottweiler Metzgerhund, meaning Rottweil butchers’ dogs, because they are descends from dogs used by the Romans to drive the herds that fed the army as it marched through Europe. Along the way, the Roman dogs bred with local dogs, and in the town of Rottweil, the result was strong dogs used by butchers to drive cattle to market. On the way home, the dogs served as protection, guarding the butcher’s proceeds from robbers. Rottweilers are slightly longer than tall, large dogs, ranging in height from 22 inches for a small female to 27 inches for a large male. They are blocky dogs with massive heads. Ears lie fairly tight to the head, hanging down somewhat. Muzzles are square and strong, but Rottweilers can be a bit drooly because of loose flews (lips). Rottweilers should always be black with tan points, and the ideal coat is quite short, dense, and a bit harsh. The Rottweiler breed often gets a bad reputation. You’ve probably heard — in one way or another — that Rotties can be incredibly aggressive, downright mean, and off-putting to other people. While these traits can certainly be true, and are perhaps a bit worse when it comes with a dog powerful enough to do damage, these traits don’t apply to most Rottweilers. The personality of every dog depends on their upbringing, how they were bred, and the personality of their parents. These ‘bad’personalities often come from poorly bred puppies that didn’t experience proper socialization. The true personality of a Rottweiler, and what they were bred to be, is a mixture of the loyal, steadfast watchdog, and the incredibly homebody. Also, despite popular belief, the Rottweiler loving is actually one of the most intelligent dog breeds in existence . As both an independent and intelligent breed, the Rottweiler requires an experienced hand for control, letting a dominant-minded dog run unchecked within the family can lead to many negative behaviors. Apart from these traits, it’s important to realize that there can be quite a lot of variation in the personality of Rottweiler’s, Some tend to be natural entertainers who love to play, while others may be much more reserved and calm. Besides, even with their dominant temperament, this breed is vulnerable to several diseases, here are some of the most common diseases related to this breed. Bloat : Gastric dilatation volvulus, also known as GDV or bloat, usually occurs in dogs with deep, narrow chests. This means the Rott is more at risk than other breeds. When a dog bloats, the stomach twists on itself and fills with gas. When a dog bloats, the stomach twists on itself and fills with gas. The twisting cuts off the blood supply to the stomach and sometimes to the spleen. Left untreated, the disease is quickly fatal, sometimes in as little as half an hour. Bone and Joint Problems : A number of different musculoskeletal problems have been reported in Rottweilers. While it may seem overwhelming, each condition can be diagnosed and treated to prevent undue pain and suffering. With diligent observation at home and knowledge about the diseases that may affect your friend’s bones, joints, or muscles, you will be able to take great care of him throughout his life. Neurologic Problems : Several neurologic diseases can afflict Rottweilers. Symptoms of neurological problems can include seizures, imbalance, tremors, weakness, or excessive sleeping. Hip dysplasia: Rottweilers are one of the breeds most affected by hip dysplasia, a genetic deformity in which the head of the femur doesn’t fit properly into the hip socket. This condition can range from mild to severe. Severe cases are extremely painful and often require surgery to correct. Even with the surgery, the dog is likely to develop arthritis as he ages. Inflammatory Bowel Disease : Inflammatory bowel disease, or IBD, is an immune system disorder common in Rotts in which the intestinal lining becomes overrun with immune system cells called lymphocytes and plasmacytes. The stomach and/or intestinal lining becomes thickened affecting his ability to absorb nutrients properly. Chronic vomiting or diarrhea is common, or symptoms may flare up suddenly and then improve again for a time. Stress, diet change, or intestinal parasites can make IBD worse. Sources: http://www.vetstreet.com/dogs/rottweiler#overview https://www.harlingenveterinaryclinic.com/services/dogs/breeds/rottweiler# Photo credit: https://en.wikipedia.org/wiki/Rottweiler https://www.goldenacresdogs.com/guard-dogs-rottweiler.html
Breed-related disease: American Bobtail

John K. Rosembert The American Bobtail is an uncommon breed of domestic cat which was developed in the late 1960s, which descends from a short-tailed kitten acquired by a couple John and Brenda Sanders during a vacation to Arizona. It is a medium to large, semi-cobby cat. Their sturdy bone structure and well-developed musculature, along with their broad chest and slightly arched back (due to longer hind than front legs), give them the appearance of a small Lynx. Their head is broad with prominent cheeks and a strong chin, and a triangular-shaped muzzle a little wider than it is long. Their eyes are big and slightly almond-shaped. Their ears, which are average sized and sit quite low on the skull, each have a small tuft of fur at the end known as “Lynx tips”. The variety with mid-length fur also have tufts of fur between the toes. The American Bobtail is devoted to family, and is very easily trained to walk on a leash. This cat breed enjoys playing with interactive cat toys, other cats, and children. The American Bobtail makes for an ideal family companion. This is a smart cat who enjoys puzzle toys, learning tricks, and playing fetch. He isn’t as vocal as some breeds, but he communicates his pleasure with chirps, clicks and trills, as well as the standard purr and meow. The American Bobtail has an adaptable nature, so he’s a good traveler. Long-distance truckers and travelers find him to be an excellent companion. The cats have also found a niche with some psychotherapists because of their loving and intuitive nature. That same adaptability and kindness makes him a good family companion and suited to a variety of lifestyles, from relaxed to rowdy. American Bobtails are generally healthy cats with no predispositions to inherited health conditions, however that doesn’t mean that every American Bobtail will never experience health problems, it’s important to note: American Bobtails with no tail may experience: Spinal Problems: The American Bobtail may be prone to spinal problem due to their short spine. Polycystic kidney disease (PKD): A condition characterized by the development of cysts on one or both kidneys. Hypertrophic cardiomyopathy: Which is the thickening of the heart muscle. Hip Dysplasia: This is rare in domestic cats, and is common in purebred cats. This occurs when the hip joint is loose, and leads to degenerative joint disease. (osteoarthritis) Symptoms include lameness that can be mild to severe. Cats generally need no surgery for hip dysplasia. Weight reduction can help reduce discomfort. Source: https://petonbed.com/american-bobtail/ https://www.thesprucepets.com/american-bobtail-full-profile-history-and-care-4705973 Photo credit: https://cattime.com/cat-breeds/american-bobtail-cats
Breed-related disease: Dachshund

The dachshund originated in Germany as a hunting dog. Though its origins can be traced as far back as the 15th century, the breed’s development really began in 17th century Germany. Called dachshunds, which translates as “badger dogs,” these short hounds did just that—they hunted badgers. Their short legs, loose skin, big chests, determination, and independence were ideal for digging, entering tunnels, and of course, fighting badgers. Their flap-down ears help keep dirt and debris out when burrowing. The Dachshund comes in three coat varieties and two sizes. The original Dachshunds were smooth coated and arose from crosses of the Bracke, a miniature French pointer, with the Pinscher. They’re all short with cute stubby legs, but Dachshunds actually come in three sizes: standard, miniature, and kaninchen (“rabbit” in German). A full grown standard Dachshund averages 15-28 lbs. while the miniature typically weighs less than 11 lbs. The kaninchen usually weighs around 8-10 lbs. The word “icon” is terribly overworked, but the Dachshund—with his unmistakable long-backed body, little legs, and big personality—is truly an icon of purebred dogdom, Dachshunds aren’t built for distance running, leaping, or strenuous swimming, but otherwise these tireless hounds are game for anything. Smart and vigilant, with a big-dog bark, they make fine watchdogs. Bred to be an independent hunter of dangerous prey, they can be brave to the point of rashness, and a bit stubborn, but their endearing nature and unique look has won millions of hearts the world over. Dachshunds, as with every BREED, have certain health issues that occur more frequently within their “genetic pool. In this article we’ll mention some of the most common health issues that are very prone to Dachshunds Dachshund Stomach Issues: it is not uncommon for Dachshund’s to experience stomach issues. Some are merely sensitive to certain foods or abrupt food changes. Others can suffer from gastroenteritis, a term referring to stomach issues resulting in inflammation of the gastrointestinal tract. Dachshunds tend to be more prone to developing hemorrhagic gastroenteritis. Liver Disease: Dachshunds are more likely than most breeds to have a liver disorder called portosystemic shunt (PSS). This is a hereditary condition in which the liver can’t effectively remove toxins from the bloodstream, Surgery is sometimes needed, but many times you can treat it with medication and a special diet. Cancer/ tumor : Dachshunds have a higher than average risk of developing cancers of the skin, fat cells, and anal sacs, this includes a particular risk of developing mast cell tumors and squamous cell carcinoma. Dachshunds have an increased risk of getting cancer. Eye Problems: Dachshunds are prone to several different eye problems. Some are extremely painful; others can cause blindness if not treated right away. Cataracts and glaucoma are common eye issues that Dachshunds may experience. Glaucoma is a very painful disease that can lead to blindness if not treated, while Cataracts are more common in older Dachshunds and can cause blindness, but surgery can restore sight in some cases. Intervertebral disk disease: conditions severe enough for hind-end paralysis are so common that Dachshunds are one of the breeds most likely to spend part of their lives in “canine wheelchairs”: wheeled carts that support the rear of the dogs. Because of their long, low-slung spines, normal canine behavior like jumping off the sofa may result in a slipped, pinched, herniated or ruptured disc Diabetes mellitus: which is caused by the failure of the pancreas to regulate blood sugar, diagnosed by the presence of the typical clinical signs (excess thirst, excess urination, excess appetite, and weight loss), a persistently high level of glucose in the blood, and the presence of glucose in the urine. Diabetes is the only common disease that will cause the blood glucose level to rise substantially in dogs. Sources: http://www.vetstreet.com/dogs/dachshund#health https://formydachshund.com/11-of-the-most-common-health-issues-in-dachshunds/ https://en.wikipedia.org/wiki/Dachshund Dachshund
Breed-related disease: Ragdolls

In the family of cat breeds, Ragdolls are among the younger siblings. The cats were first developed by breeder Ann Baker who wanted to develop a beautiful cat with a loving, gentle personality, and she started with domestic longhairs of unknown ancestry. Josephine, the foundation cat, was white with Siamese-type markings, and in her genes she carried a seal mitted or black tuxedo pattern. The Ragdolls of today descend from Josephine and her son, Daddy Warbucks, as well as other unknown domestic longhair males. The Cat Fanciers Association began registering Ragdolls in 1993, and they achieved championship status in 2000. Ragdolls are sometimes nicknamed “puppy cats” because of the way they follow their people from room to room, sometimes even taking your privacy from the bathroom. Unlike many cats, Ragdolls are notable for collapsing into the arms of anyone who holds them, even if they are cradled on their back. They love their people, greeting them at the door, following them around the house, and leaping into a lap or snuggling in bed whenever given the chance. They often learn to come when called or to retrieve toys that are thrown for them. All cats have the potential to develop genetic health problems, both pedigreed cats and mixed-breed cats have varying incidences of health problems that may be genetic in nature. Problems that may affect the Ragdoll include the following: Hypertrophic cardiomyopathy : which is a condition in which a portion of the heart becomes thickened without an obvious cause. This results in the heart being less able to pump blood effectively. Symptoms vary from none to feeling tired, leg swelling, and shortness of breath and even sudden death. Blood clots: Ragdolls can be susceptible to blood clots in the arteries. Symptoms include difficulty breathing, loss of appetite, lethargy and depression. Some cats may also faint. Treatment is available, but it is imperative to see a vet as soon as these symptoms appear. Dilated and restricted cardiomyopathy : Dilated cardiomyopathy is caused by the dilation of the heart muscles. Restricted cardiomyopathy is caused by weakened elasticity of the heart muscles. Both can be fatal and need to be detected and treated as soon as possible. Sources: http://www.vetstreet.com/cats/ragdoll#health https://cattime.com/cat-breeds/ragdoll-cats#/slide/1 https://bowwowinsurance.com.au/cats/cat-breeds/ragdoll/
Breed-related disease: Poodle

Poodles are believed to have originated in Germany, though they have been known as French dogs for many years. Their name is derived from the German word pudel, meaning “to splash in water.” Standard poodles are considered the oldest form of this breed. Their history of use as retrievers and water dogs led to the well-known poodle haircut, which was designed to protect joints from cold water temperatures. The breed share a square outline, with a long, elegant neck and a straight back. The tail is docked, but not short, so it can wave gaily. Poodles tend to have a leggy appearance and a long muzzle combined with dropped ears. They move with a springy, lively gait. The coat of the poodle is its crowning glory. Dogs competing in the breed ring must have a specific clip, with areas of extravagant hair coupled with skin tight clipping, these clips actually developed for a reason: they provided thick coat over the joints and chest to keep the dog warm while working in cold water. Intelligent, loving, loyal, and mischievous are four words Poodle enthusiasts commonly use to describe the breed’s personality. Poodles are among the smartest of breeds, but that intelligence can translate into stubbornness. Even so, they can make wonderful therapy dogs. Their empathetic nature and joy in engaging with people make them naturals for visiting with people in nursing homes, hospitals, and schools . Poodles are active dogs, but the smaller dogs need less room and less exercise. Toy and Miniature Poodles are often the companions of people who are less active and can be extremely happy as lap dogs and TV-watching buddies. Just be sure their busy minds have enough to keep them out of mischief. Poodles love to learn and want to please. Trick-training suits their heritage as circus dogs quite well. Teach them to pick up the newspaper, carry a bottle to the recycling bin, and bring your slippers . All dogs have the potential to develop genetic health problems, just as all people have the potential to inherit a particular disease, Poodles are generally considered to be a very sturdy breed with few health issues. Addison’s Disease : Also known as hypoadrenocorticism, this extremely serious condition is caused by an insufficient production of adrenal hormones by the adrenal gland. Most dogs with Addison’s disease vomit, have a poor appetite, and lethargy. Because these signs are vague and can be mistaken for other conditions, it’s easy to miss this disease as a diagnosis until it reaches more advanced stages. Gastric Dilatation-Volvulus : Commonly called bloat, which occurs when gas gets trapped inside a dog’s stomach. The stomach twists as much as 180 degrees, stopping the flow of digestion and causing the gas to build up pressure. It’s an incredibly painful disorder with a 20% mortality rate even with surgical intervention. Deep-chested breeds like the standard Poodle or Great Dane are especially prone to experiencing bloat. Hip Dysplasia : A dog’s hip operates on a ball-and-socket joint. When the socket is over- or under-developed, or when the ligaments holding the two together are weak, the ball can become dislodged. This constant dislocation and relocation will wear down the joint’s integrity and cause hip dysplasia. Hypothyroidism: Hypothyroidism is caused by an under active thyroid gland. It’s thought to be responsible for conditions such as epilepsy, hair loss, obesity, lethargy, hyperpigmentation, pyoderma and other skin conditions. Epileptic : Epileptic seizures in dogs are as shocking for canines as they are for humans. Dogs will often seem confused or panicked about what’s happening, and the sight of your dog seizing can be terrifying to watch. When this happens, you need to remain calm and focus on helping your dog. https://dogtime.com/dog-breeds/poodle#/slide/1 https://en.wikipedia.org/wiki/Poodle
Feline Calicivirus Review: Biology, Risks, and Care

Table of Contents 1. Introduction: Feline Calicivirus in Veterinary Practice 1.1 Background Feline Calicivirus (FCV) remains one of the most clinically significant viral pathogens affecting domestic cats, particularly as a leading cause of upper respiratory tract infections (URTIs). Its impact is amplified by the virus’s intrinsic biological properties: FCV exhibits high genetic variability, a remarkable ability to persist in chronically infected carriers, and environmental stability that enables sustained circulation within shelters, colonies, and multi-cat households. These features contribute not only to recurrent outbreaks but also to efficient viral maintenance within feline populations worldwide. From a virological standpoint, FCV is a small, non-enveloped, icosahedral virus, measuring approximately 30–40 nm in diameter and harboring a single-stranded positive-sense RNA genome of roughly 7.7 kb. Its use of junctional adhesion molecule-1 (JAM-1) as a cellular receptor facilitates viral entry and dissemination. Infection typically begins following exposure through the nasal, oral, or conjunctival routes, with the oropharynx serving as the primary site of replication. Viral amplification here drives epithelial necrosis, leading to the characteristic oral ulcerations most commonly identified along the margins of the tongue. Given the combination of widespread prevalence, substantial morbidity, and occasional highly virulent systemic outbreaks, a consolidated review of FCV’s structure, replication biology, epidemiology and clinical behavior remains essential for contemporary veterinary practice. 1.2 Objectives This article aims to synthesize current evidence from molecular virology, clinical epidemiology and field management to guide veterinary professionals, shelter medicine practitioners and cattery managers. Summarize evidence-based findings on FCV structure, replication and pathogenesis.A molecular understanding of FCV underpins rational approaches to diagnosis, prevention and therapeutic intervention. Particular focus is placed on capsid architecture, genomic organization, antigenic variability and the early host–virus interactions that shape clinical outcomes. Provide veterinarians and cattery managers with practical prevention and care strategies.In high-density environments, controlling FCV transmission requires a layered approach that combines:• vaccination programs,• minimizing population stress and overcrowding,• rigorous hygiene and environmental disinfection, and• timely clinical management of affected cats. Although vaccination remains central to disease mitigation, it typically does not prevent infection or viral shedding, and breakthrough infections continue to occur. Effective clinical management therefore relies heavily on supportive measures such as intravenous fluid therapy for dehydration, nonsteroidal anti-inflammatory drugs for pyrexia and oral pain, and targeted antibiotics for secondary bacterial complications. Highlight key clinical risks, including oral ulceration, FCV-associated lameness and virulent systemic disease (VSD). Oral Ulceration:A hallmark of classical FCV infection, especially in kittens, appearing after an incubation period of 2–10 days. It is frequently accompanied by sneezing and serous nasal discharge. FCV-Associated Lameness:Characterized by acute synovitis with joint effusion and synovial membrane thickening. This syndrome may arise days to weeks after respiratory signs or following vaccination. • Virulent Systemic Disease (VSD):A rare, highly pathogenic phenotype with reported mortality rates up to 67 percent. VSD is marked by systemic inflammatory response syndrome, disseminated coagulopathy and multi-organ failure. Clinically, affected cats exhibit severe URTI signs followed by cutaneous ulcerations, alopecia of the extremities, broncho-interstitial pneumonia and necrosis of major organs including the liver, spleen and pancreas. Management requires intensive supportive care, often incorporating corticosteroids and interferon. 2. Viral Structure and Molecular Biology Feline Calicivirus (FCV) belongs to the Caliciviridae family, a group of small, non-enveloped RNA viruses characterized by compact genomes and efficient replication strategies. The structural and molecular features of FCV underpin its clinical behavior, including its ability to persist, diversify, and evade immune surveillance in feline populations. 2.1 Virion Architecture FCV is a non-enveloped, icosahedral virus measuring 30–40 nm in diameter. Its capsid is considered “naked”, reflecting the absence of a lipid envelope. The virion is composed of a single capsid protein, with a precursor mass of 65–66 kDa, which is later processed into the major structural protein VP1. This protein forms the characteristic icosahedral shell that encases the viral RNA genome. 2.2 Genome Organization The genome of FCV consists of a single-stranded, positive-sense RNA molecule of approximately 7.7 kb, organized into three Open Reading Frames (ORFs): ORF1 – Non-structural Polyprotein Encodes a 200 kDa polyprotein that undergoes proteolytic cleavage to produce six mature non-structural proteins, essential for RNA replication and virion assembly. ORF2 – Capsid Precursor (preVP1) Encodes a 73 kDa capsid precursor (preVP1).• Undergoes rapid cleavage during maturation to yield the 60 kDa VP1 capsid protein.• Subdivided into regions A–F; among these, the E-region determines antigenicity and contributes to formation of the P2 subdomain, a key external protrusion involved in receptor interaction and immune recognition. ORF3 – Minor Structural Protein VP2 Encodes VP2, a 12 kDa protein (106 amino acids) that, although less abundant, is essential for producing infectious virions and supports VP1 stability during assembly. https://share.google/unsumbG6JXsez5x1R 2.3 Replication Cycle FCV replication proceeds through the synthesis of: A 7.7 kb genomic RNA (positive-sense)• A 2.4 kb subgenomic RNA, which serves as the template for capsid protein translation Viral entry is mediated by junctional adhesion molecule-1 (JAM-1), identified as the functional receptor during in vitro studies. Once inside the host cell, FCV induces a characteristic cytopathic effect (CPE)—notably cell rounding and membrane blebbing. A central mechanism of viral dominance is the shut-off of host protein synthesis, accomplished through cleavage of eIF4G, a critical eukaryotic initiation factor. This redirection enables preferential translation of viral RNA and efficient progeny production. 3. Epidemiology 3.1 Global Distribution Feline Calicivirus (FCV) was first isolated from the gastrointestinal tract of cats in New Zealand (Fastier, 1957). Since that initial discovery, FCV has been recognized as a globally widespread pathogen, circulating in domestic and free-roaming feline populations across continents. Its prevalence is particularly high in high-density environments, such as multi-cat households, shelters, and breeding colonies. Studies consistently report 25–40 percent infection rates among cats in colonies and shelters (Wardley et al. 1974, Bannasch & Foley 2005). The combination of environmental persistence, antigenic diversity, and efficient cat-to-cat transmission ensures FCV remains an endemic viral pathogen in most feline communities worldwide. 3.2 Transmission and Persistence FCV transmission occurs predominantly through oral, nasal, or conjunctival exposure. Direct contact with secretions, as well as indirect exposure through contaminated fomites, facilitates rapid spread—particularly in
Canine blood-typing
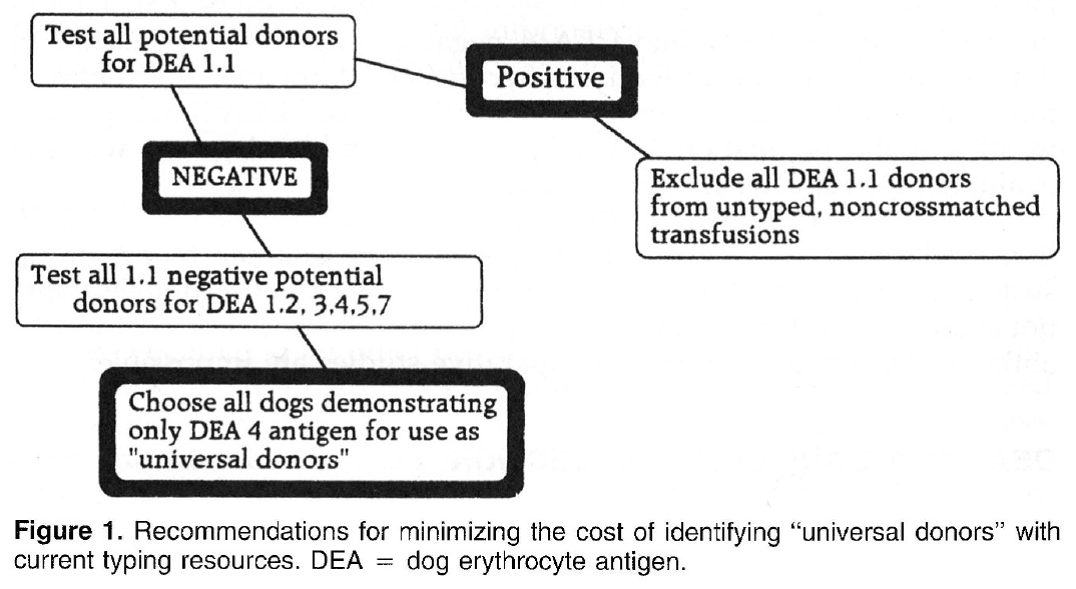
Canine blood-typing Andy Pachikerl, Ph.D Introduction: Dog erythrocyte antigens are responsible for initiating approximately 70% to 80% of immune-mediated transfusion reactions in the dog. As with other species, the red blood cell antigens found in the dog have various immunogenicities. In health, these antigens are participants in cell recognition-self versus nonself. In disease, they may serve as antigens for antibody or markers in disease occurrence. Little is known about their biochemical properties. Currently their description is reliant on polyclonal antibody serology. This reliance has limited the progress of transfusion practice in the dog. Historically, the study of canine blood groups and their importance in transfusion began in the 1600s through a physician, Richard Lower. He is credited with the first canine-to-canine transfusion. The efforts of doctors Lower and Denis in heterologous transfusion using lamb, dog, and human subjects introduced the basic transfusion premise “like transfuses like.” In 1910, Von Dungem and Hirszfeld documented the presence of four hemolysins and agglutinins based on canine alloimmunization (Swisher & Young, 1961). Further work by Ottenburg, Kaliski, and Friedman in 1913 confirmed these findings. From 1937 to 1949, Wright, Whipple, and Eyquem further defined the presence of six canine blood groups (Colling & Saison, 1980). However, not until 1961 was the importance of these antigens in transfusion and disease investigated by Swisher, Young, and Trabold (Swisher, et al., 1962). To date, the work submitted by Swisher and Young remains the most current published information of the importance of canine blood groups in transfusion (Swisher, 1954; Swisher, et al., 1962; Young, et al., 1951). Additional blood groups have been identified by Rubenstein (1968), Suzuki/5 Colling and Saison (Colling & Saison, 1980; Colling & Saison, 1980), and Symons and BelLl9 (Symons & Bell, 1992). Of this latter group, only the antigen first noted by Rubenstein (Colling & Saison, 1980) was evaluated in regard to transfusion significance by Bull (Bull, 1976). The importance of canine blood groups in veterinary transfusion medicine is based on three factors: the incidence of the antigen in the dog population, the incidence of naturally occurring antibody within the population, and the effect of the antibody against the antigen in vivo. Current blood typing schemes identify six erythrocyte antigens with possible importance. The dog erythrocyte system Blood groups are defined by glycolipids and glycoproteins on the surface of the red blood cell membrane. Current blood typing schemes identify six dog erythrocyte antigens (DEAs): 1.1, 1.2, 3, 4, 5, and 7 (Table 1). Blood groups are independently inherited. Simple Mendelian laws of dominance govern their inheritance. These antigens are defined by using polyclonal antibodies generated through canine alloimmunization. Polyclonal antibody recognition may be dependent on multiple recognition sites to define the “antigens” currently accepted. Biochemically, little is known about the DEA system. Table 1. Dog erythrocyte antigens established as international standards: classification, occurrence, and significance This blood group system has been defined with multiple alleles. They include the antigens 1.1, 1.2, 1.3, and a null type. An individual dog may show only one of the four phenotypes. Family studies suggest a Mendelian type of autosomal dominance. Table 2 describes the current phenotypic and genotypic information on this blood group system. 1.1- and 1.2-positive dogs have been studied for transfusion significance. Naturally occurring antibody to these alleles has not yet been found. Therefore, first-time transfusion reactions do not occur. However, if a negative dog is exposed to 1.1- positive erythrocytes, a strong hemolysin can result. On second exposure, an immune-mediated hemolytic transfusion reaction results causing removal of transfused cells in less than 12 hours. Hemoglobinuria and hyperbilirubinemia frequently occur. In addition to uncross matched, untyped transfusion, pregnancy can cause production of antibody against DEA 1.1 25% of the time. For these reasons 1.1-positive dogs are excluded as transfusion donors. 1.2-positive dogs can cause a problem as both the transfusion donor and recipient. A previously sensitized negative type dog undergoes permanent red blood cell removal and loss 12 to 24 hours after the administration of 1.2-positive red blood cells. Thus, 1.2-positive dogs are poor erythrocyte donors. If a 1.2-positive dog is sensitized with DEA 1.1 red blood cells, it will produce a potent anti-DEA 1.1 antibody. Administration of DEA 1.1 red blood cells to a sensitized 1.2 dog results in an immediate hemolytic transfusion reaction. Therefore, 1.2-positive dogs are at risk after sensitization for immediate transfusion. 1.3-positive dogs have not been evaluated for transfusion significance. Future study is limited because of the unavailability of typing sera for DEA 1.3. DEA 7 This red blood cell antigen is the most controversial among the six antigens discussed. Published reports of naturally occurring antibody to this antigen suggest that this antibody has a natural prevalence as high as 50% in DEA 7-negative dogs. Recent reports by Giger fail to support the presence of naturally occurring anti-DEA 7. Observations by the author suggest that naturally occurring antibody does exist in 20% to 50% of all DEA 7-negative dogs. However, the naturally occurring antibody is quite weak, rarely producing a titter greater than 1:8. In the presence of naturally occurring antibody, as in the cat, immunemediated transfusion reaction can occur during a first transfusion. Sensitized DEA 7-negative dogs, when transfused with DEA 7-positive erythrocytes show a delayed transfusion reaction. Hemolysis does not occur; however, an irreversible sequestration and loss of red blood cells occurs in 72 hours. This type of delayed transfusion reaction is only significant if the regenerative ability of the transfusion recipient is compromised. Because of the presence of naturally occurring antibody in the DEA 7-negative population and because of the delayed loss of erythrocytes in sensitized dogs, DEA 7-positive dogs are not recommended as donors. DEA3 This antigen has not been considered significant because of its low incidence in the dog population of the United States. However, recent evaluation of DEA type by breed suggests that it may be more important. Only 6% of the general population has DEA 3-positive cells. Yet 23% of the Greyhounds typed from 1990 to
