Introduction to Feline Hypertrophic Cardiomyopathy
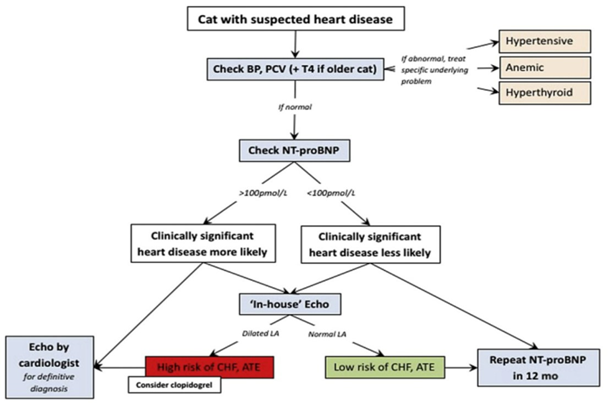
Maigan Espinili Maruquin It is important to be aware that some of the diseases your pets may have are actually inherited. In cats, there are myocardial diseases that can be breed- related. The most common myocardial disease in cats is Hypertrophic cardiomyopathy (HCM), wherein abnormal thickening of the walls of the left ventricle (LV) is observed [1]. First time described in cats in 1977 [2], it has been reported to have a prevalence of around 14.7% in apparently healthy cats [3-5]. In humans, the HCM is considered a genetic disease [6-8], whereas occurrences of the disease were observed in mix- breeds [9], Persian [10], and American shorthair cats [11], while an HCM caused by mutation was identified in Maine coon [12] and ragdoll [13]. The HCM are diagnosed at mean of 5-7 years, although all ages can get the disease [6]. On the other hand, some cat breeds including Maine Coons [14]; Sphynx [15], and Ragdoll [16] were reported on earlier onset of under 2 years old [3]. Cats that are diagnosed with HCM are also recorded to develop congestive heart failure (CHF), arterial thromboembolism (ATE), or sudden cardiac death (SCD) [1, 17, 18]. Clinical Presentation When cats visit the clinics, routine veterinary examinations are conducted, and during auscultation, signs like arrhythmias, gallop sounds, or murmurs can be detected [6, 19, 20]. Respiratory distress is a manifestation of heart failure in diseased cats, whereas, some cats display hypothermia and pre-renal azotemia. On the other hand, the murmurs in cats may vary in intensity form moment to moment, and are commonly associated with dynamic and labile phenomena [6]. Diagnosis Fig. 1. Approach to the asymptomatic cat with suspected heart disease. BP, blood pressure; PCV, packed cell volume; T4, thyroxine [1] The feline HCM are primarily diagnosed on echocardiographic examination, which recognizes basic patterns that are intuitive [21], with ventricular wall thickness that is equal to or exceed 6 mm [6, 22]. Respiratory distress is reported to display left atrial enlargement. However, echocardiographic examination has limitations [1] and there is no definitive, gold-standard to diagnose HCM, unless there is a hypothetical and flawless molecular or genetic testing [6]. The LV wall thickness has no exact value allowable, and body weight can affect its thickness [1]. An increase of cTn-I in plasma concentration indicates its sensitivity and specificity as a biomarker to provide myocardial damage severity and prognosis information. On the other hand, the N-terminal pro B-type natriuretic peptide (NT-proBNP) assay may provide ongoing myocardial stress, however, full cardiac evaluation shall be performed to detect its cause of elevation [1]. Myocyte enlargement and interstitial fibrosis were observed, along with disorganized spatial arrangement of myocytes in histopathological examination [3, 23] Genetic testing for single point mutation that affects MYBPC3 in Maine coon cats (A31P) [12] and ragdolls (R820W) [13] are commercially available. Autosomal dominant inheritance were reported in both breeds [1]. Therapy and Management For asymptomatic cats with HCM, diltiazem or beta-blockers were reported to improve physical condition. Meanwhile, Diltiazem is administered at three times a day as a licensed formulation in UK to manage cases of HCM [21]. In a study conducted by Rishniw, M. and P.D. Pion in 2011, participatiing clinicians used furosemide for evident CHF, and most of them also used and ACEIs, while for cases with substantial dynamic LVOT obstruction, β-blockers were used by most [24]. Altering the progression of HCM in the pre- or subclinical stage is an approach that is ideal in the absence of safe and efficient therapy [1]. References Luis Fuentes, V. and L.J. Wilkie, Asymptomatic Hypertrophic Cardiomyopathy: Diagnosis and Therapy. Veterinary Clinics: Small Animal Practice, 2017. 47(5): p. 1041-1054. Tilley, L.P., et al., Primary myocardial disease in the cat. A model for human cardiomyopathy. Am J Pathol, 1977. 86(3): p. 493-522. Gil-Ortuño, C., et al., Genetics of feline hypertrophic cardiomyopathy. 2020. 98(3): p. 203-214. Paige, C.F., et al., Prevalence of cardiomyopathy in apparently healthy cats. J Am Vet Med Assoc, 2009. 234(11): p. 1398-403. Payne, J.R., D.C. Brodbelt, and V. Luis Fuentes, Cardiomyopathy prevalence in 780 apparently healthy cats in rehoming centres (the CatScan study). J Vet Cardiol, 2015. 17 Suppl 1: p. S244-57. Abbott, J.A., Feline Hypertrophic Cardiomyopathy: An Update. Veterinary Clinics: Small Animal Practice, 2010. 40(4): p. 685-700. Maron, B.J., et al., American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy. A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines. J Am Coll Cardiol, 2003. 42(9): p. 1687-713. Maron, B.J., Hypertrophic cardiomyopathy: a systematic review. Jama, 2002. 287(10): p. 1308-20. Kraus, M.S., C.A. Calvert, and G.J. Jacobs, Hypertrophic cardiomyopathy in a litter of five mixed-breed cats. J Am Anim Hosp Assoc, 1999. 35(4): p. 293-6. Marin L, V.S., Boon J, et al., Left ventricular hypertrophy in a closed colony of Persian cats [abstract]. J Vet Intern Med 1994. 8:143. Meurs KM, K.M., Towbin J, et al., Familial systolic anterior motion of the mitral valve and/or hypertrophic cardiomyopathy is apparently inherited as an autosomal dominant trait in a family of American shorthair cats. J Vet Intern Med, 1997. 11:138. Meurs, K.M., et al., A cardiac myosin binding protein C mutation in the Maine Coon cat with familial hypertrophic cardiomyopathy. Hum Mol Genet, 2005. 14(23): p. 3587-93. Meurs, K.M., et al., A substitution mutation in the myosin binding protein C gene in ragdoll hypertrophic cardiomyopathy. Genomics, 2007. 90(2): p. 261-4. Kittleson, M.D., et al., Familial hypertrophic cardiomyopathy in maine coon cats: an animal model of human disease. Circulation, 1999. 99(24): p. 3172-80. Chetboul, V., et al., Prospective echocardiographic and tissue Doppler screening of a large Sphynx cat population: Reference ranges, heart disease prevalence and genetic aspects. Journal of veterinary cardiology : the official journal of the European Society of Veterinary Cardiology, 2012. 14. Borgeat, K., et al., The influence of clinical and genetic factors on left ventricular wall thickness in Ragdoll cats. J
Feline Hyperthyroidism

Sushant Sadotra Introduction: One of the most common diseases in middle-aged and older cats is hyperthyroidism. An increase in the production of thyroid hormones, i.e., T4 and T3, is the primary cause of this disorder. The enlarged thyroid gland in the neck region of the cat is the most common visible sign identifying hyperthyroidism. This enlargement is a non-cancerous tumor known as an adenoma. However, in some rare cases, it can also be caused by malignant tumors known as thyroid adenocarcinomas. Hyperthyroidism, also called thyrotoxicosis, increases the metabolic rate in an animal’s body because of high circulating thyroid hormone and often causes secondary problems by affecting all of the organs in the body. The reason for feline hyperthyroidism is unfamiliar. However, deficiencies or excesses of some elements in the diet and thyroid-disrupting could be responsible for the onset of hyperthyroidism. Hyperthyroidism is rare in dogs. However, if it occurs, it is primarily because of thyroid carcinoma. This contrasts with the case in hyperthyroid cats, where less than 5% of a thyroid tumor is carcinoma. Clinical signs: Cats’ most common clinical signs of hyperthyroidism are weight loss, increased appetite, vomiting, diarrhea, increased fecal volume, hyperexcitability, polydipsia, polyuria, enlargement of the thyroid gland, cardiomegaly, and congestive heart failure. Diagnosis A high thyroid hormone concentration in serum is the primary indication of hyperthyroidism. Therefore measuring serum total T4 concentration is the standard procedure that can confirm the diagnosis of hyperthyroidism in cats. In 5% – 10% of cases, it is also seen that cats so have normal T4 levels. It could be an indication of early or mild hyperthyroidism. Suppression of a high total T4 level to within reference range limits can also be caused by a nonthyroidal illness concurrent with hyperthyroidism. High free T4 concentration, medical history, and physical examination diagnose hyperthyroidism in cats with normal T4 levels. Treatment Radioiodine Therapy The radioiodine can be concentrated within the thyroid gland, where it targets the tumor by selectively irradiating and destroying hyper-functioning tissue. Radioactive iodine therapy is a simple, effective, and safe treatment for cat hyperthyroidism. Thyroidectomy Unilateral thyroid tumors can be easily treatable with surgical thyroidectomy without requiring thyroxine supplementation. Thyroidectomy can also be used for bilateral thyroid tumors. However, to avoid postoperative hypocalcemia, the functioning of the parathyroid gland must be preserved. After complete thyroidectomy, thyroxine should be administered for one to two days. Vitamin D and calcium treatment are also indicated if iatrogenic hypoparathyroidism develops. Chronic administration of an antithyroid drug An antithyroid drug acts by blocking thyroid hormone synthesis. Methimazole, carbimazole, and propylthiouracil are some of the most commonly used antithyroid drugs that are used to control hyperthyroidism. An initial dose of methimazole is 2.5 mg to 5 mg and is divided into two equal amounts to be given daily. Propylthiouracil has shown some adverse effects (hemolytic anemia and thrombocytopenia) and therefore is not recommended in cats. In less than 5% of treated cats, methimazole may have adverse effects such as agranulocytosis and thrombocytopenia. Besides lowering the circulating T4 concentration, cardiovascular signs such as tachycardia, tachypnea, hypertension, and hyperexcitability are often treated using β-adrenoceptor blocking agents such as propranolol and atenolol. Another strategic drug that inhibits the conversion of peripheral T4 to T3 is the oral cholecystographic agents such as ipodate, iopanoic acid, and diatrizoate meglumine. Lifelong nutritional therapy A diet with iodine levels below the minimum daily requirement is mainly prescribed for cats that are not suitable as a candidate for surgery or radioiodine therapy or in cats that develop adverse effects from oral medication. Compared to cats with severe hyperthyroidism, this nutritional therapy is more effective if the cat has a moderate increase in T4 levels. Hill’s® y/d Feline Thyroid HealthTM is one of the prescription diets available in the market with severely restricted iodine levels. The therapy can only control but not wholly treat hyperthyroidism. Also, cats on an iodine-deficient diet must not eat any other diet or food. If the diet is stopped, a setback will occur, and the therapy will be ineffective in regulating hyperthyroidism. References Vaske, Heather H et al. “Diagnosis and management of feline hyperthyroidism: current perspectives.” Veterinary medicine (Auckland, N.Z.) vol. 5 85-96. 20 Aug. 2014, doi:10.2147/VMRR.S39985 Carney, Hazel C et al. “2016 AAFP Guidelines for the Management of Feline Hyperthyroidism.” Journal of feline medicine and surgery vol. 18, 5 (2016): 400-16. doi:10.1177/1098612X16643252 Mark E. Peterson. Hyperthyroidism in Animals. Last full review/revision Jul 2019 | Content last modified Oct 2020. MSD MANUAL Veterinary Manual.
